Relationship between influencing factors of operation time and postoperative complications in hand-assisted laparoscopic living donor nephrectomy
-
摘要:
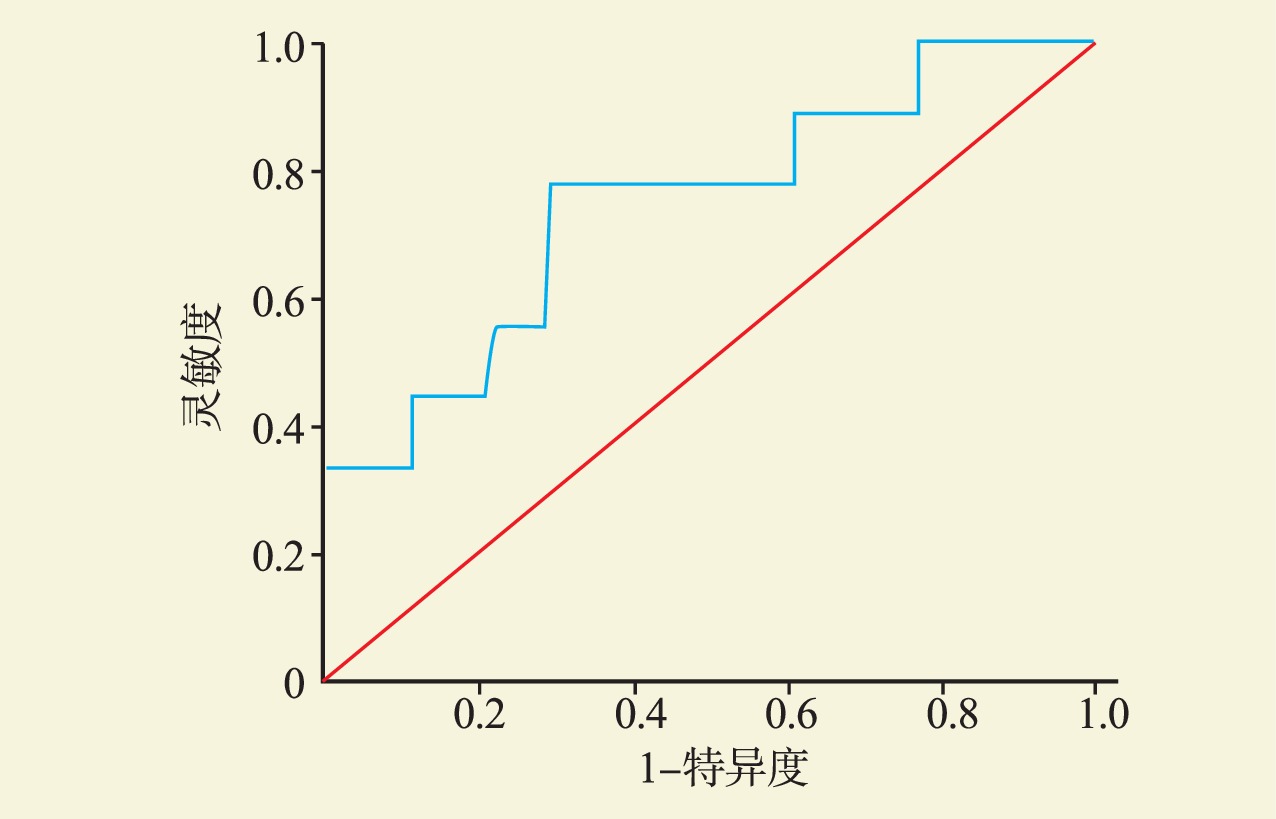
目的 探究手助腹腔镜下活体供肾切取手术时间的影响因素,并探究其与术后并发症严重程度间的关系。 方法 回顾性分析91例行手助腹腔镜下活体供肾切取术的供者的临床资料,分析供者术前基线资料与手术时间之间的相关性,研究手术时间与术后并发症的关系并确定手术时间的阈值。 结果 肾动脉数量多、肾周脂肪及肾脏后侧脂肪较厚、罹患代谢综合征、梅奥粘连概率(MAP)评分及Clavien-Dindo评分较高均会导致手术时间延长。通过分析受试者工作特征(ROC)曲线发现,当手术时间≥138 min时,供者术后并发症的发生率显著升高(P<0.05)。 结论 对于具有多支肾动脉、肾周及肾脏后侧脂肪厚度较厚、罹患代谢综合征、MAP评分及Clavien-Dindo评分较高的供者,可选择手术经验更为丰富的医师,做好充分的术前准备并在术后予以密切关注,以及时发现术后并发症并降低并发症的严重程度,改善供者预后。 -
关键词:
- 手助腹腔镜 /
- 活体供者 /
- 肾切除术 /
- 梅奥粘连概率评分 /
- Clavien-Dindo评分 /
- 受试者工作特征(ROC) /
- 脂肪厚度 /
- 代谢综合征
Abstract:Objective To identify the influencing factors of operation time of hand-assisted laparoscopic living donor nephrectomy, and to analyze the relationship between influencing factors and the severity of postoperative complications. Methods Clinical data of 91 donors who underwent hand-assisted laparoscopic nephrectomy were retrospectively analyzed. The correlation between preoperative baseline data of donors and operation time was analyzed. The relationship between operation time and postoperative complications was assessed and the threshold of operation time was determined. Results Multiple donor renal arteries, thick perirenal and posterior renal fat, metabolic syndrome, high Mayo adhesive probability (MAP) score and Clavien-Dindo score prolonged the operation time. By analyzing the receiver operating characteristic (ROC) curve, we found that when the operation time was ≥138 min, the incidence of postoperative complications of donors was significantly increased (P<0.05). Conclusions For donors with multiple renal arteries, thick perirenal and posterior renal fat, metabolic syndrome and high MAP score and Clavien-Dindo score, experienced surgeons should be selected to make adequate preoperative preparation and pay close attention after surgery, so as to timely detect postoperative complications and reduce the severity of complications, enhance clinical prognosis of the donors. -
表 1 供者术前基线资料对手术时间的影响分析
Table 1. Analysis of the influence of preoperative baseline data of donors on operation time
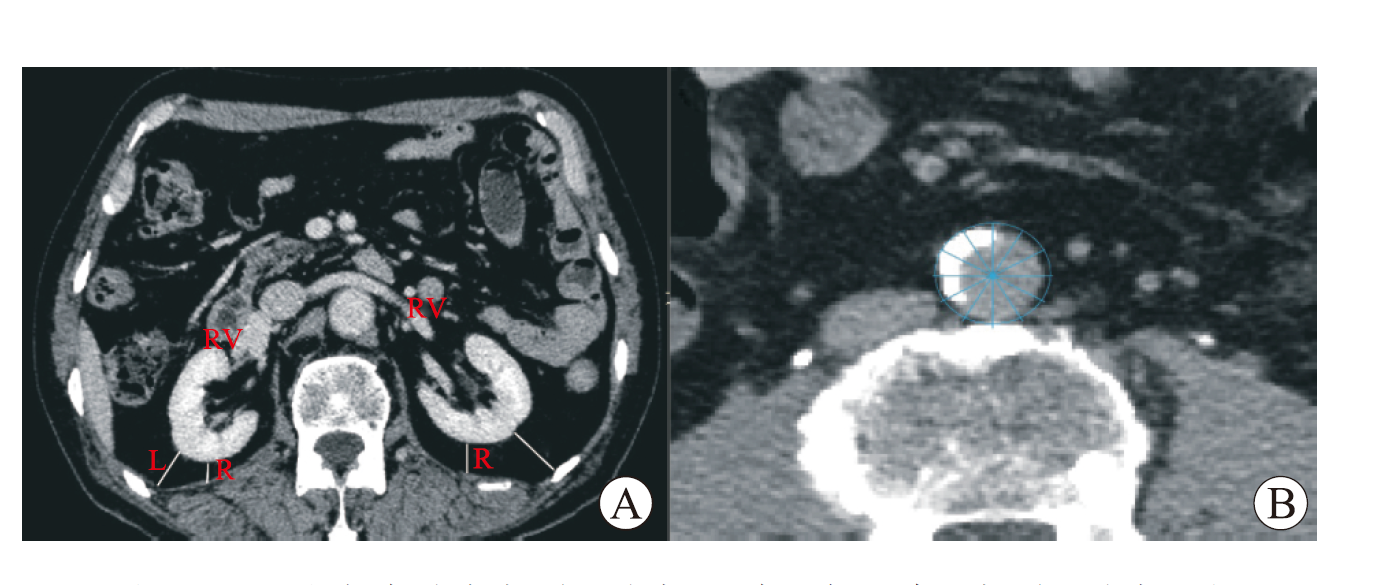
变量 n 数值 相关系数 P值 年龄[M(P25, P75),岁] 91 53(50,57) 0.012 0.909rs 男性[n(%)] 91 29(32) −0.018 0.264rs BMI($ \stackrel{-}{\mathit{x}}\pm \mathit{s} $,kg/m2) 91 24.4±2.8 0.039 0.716r 美国麻醉医师协会分级[n(%)] 91 0.710 0.945rs Ⅰ级 20(22) Ⅱ级 70(77) Ⅲ级 1(1) 吸烟史[n(%)] 91 20(22) −0.743 0.458rs 高血压史[n(%)] 91 13(14) 0.140 0.183rs 心血管疾病史[n(%)] 91 4(4) −0.015 0.483rs 总胆固醇($ \stackrel{-}{\mathit{x}}\pm \mathit{s} $,mmol/L) 91 4.6±1.0 −0.109 0.314 r 甘油三酯[M(P25, P75),mmol/L] 91 1.3(0.9,1.7) 0.084 0.435rs 代谢综合征[n(%)] 91 10(11) 0.235 0.027rs 术前血清肌酐($ \stackrel{-}{\mathit{x}}\pm \mathit{s} $,μmol/L) 91 63±11 0.204 0.053r 供肾长度[M(P25, P75),cm] 91 11.0(10.0,11.5) 0.136 0.203rs 供肾体积[M(P25, P75),cm³] 91 141.7(125.4,166.4) 0.020 0.854rs 肾动脉数量[n(%)] 91 9.537 0.002rs 1 76(84) 2 14(15) 3 1(1) 皮下脂肪厚度($ \stackrel{-}{\mathit{x}}\pm \mathit{s} $,cm) 91 2.3±0.8 −0.054 0.634r 肾周脂肪厚度[M(P25, P75),cm] 91 1.0(0.7,1.6) 0.328 0.002rs 肾脏前侧脂肪厚度[M(P25, P75),cm] 91 0.5(0.3,0.8) 0.118 0.286rs 肾脏后侧脂肪厚度[M(P25, P75),cm] 91 0.7(0.3,1.1) 0.216 0.049rs MAP评分[n(%)] 91 12.870 0.029rs 0 64(70) 1 23(25) 2 2(2) 3 0 4 2(2) 腹主动脉钙化[n(%)] 91 16(18) 0.067 0.545rs Clavien-Dindo评分[n(%)] 91 0.269 0.010rs 0 82(90) 1 2(2) 2 5(5) 3 1(1) 4 1(1) 注:当相关系数为正值时,因变量越大,手术时间越长;相反,当相关系数为负值时,因变量越大,手术时间越短。r表示采用Pearson相关性检验,rs表示采用Spearman相关性检验。 -
[1] 田野, 张磊, 解泽林, 等. 经腹膜后入路腹腔镜活体供肾切取技术的改良及效果观察[J]. 中华器官移植杂志, 2012, 33(10): 580-583. DOI: 10.3760/cma.j.issn.0254-1785.2012.10.002.TIAN Y, ZHANG L, XIE ZL, et al. Improvement and effect of retroperitoneal laparoscopic living donor nephrectomy[J]. Chin J Organ Transplant, 2012, 33(10): 580-583. DOI: 10.3760/cma.j.issn.0254-1785.2012.10.002. [2] 侯雨时, 吕竟成, 侯海军, 等. 围手术期缓解活体肾移植供者术后疼痛的研究进展[J]. 国际外科学杂志, 2023, 50(2): 132-139. DOI: 10.3760/cma.j.cn115396-20220130-00036.HOU YS, LYU JC, HOU HJ, et al. Research progress of perioperative pain relief in living donor kidney transplantation[J]. Int J Surg, 2023, 50(2): 132-139. DOI: 10.3760/cma.j.cn115396-20220130-00036. [3] 朱一辰, 侯雨时, 吕竟成, 等. 术中切口联合局部麻醉改善后腹腔镜活体供肾切取术后疼痛的研究[J]. 国际外科学杂志, 2021, 48(12): 829-833,f4. DOI: 10.3760/cma.j.cn115396-20211013-00398.ZHU YC, HOU YS, LYU JC, et al. Intraoperative incision combined with local anesthesia to improve postoperative pain after laparoscopic live donor nephrectomy[J]. Int J Surg, 2021, 48(12): 829-833,f4. DOI: 10.3760/cma.j.cn115396-20211013-00398. [4] SU LM, RATNER LE, MONTGOMERY RA, et al. Laparoscopic live donor nephrectomy: trends in donor and recipient morbidity following 381 consecutive cases[J]. Ann Surg, 2004, 240(2): 358-363. DOI: 10.1097/01.sla.0000133351.98195.1c. [5] WINDISCH OL, MATTER M, PASCUAL M, et al. Robotic versus hand-assisted laparoscopic living donor nephrectomy: comparison of two minimally invasive techniques in kidney transplantation[J]. J Robot Surg, 2022, 16(6): 1471-1481. DOI: 10.1007/s11701-022-01393-x. [6] DAGNÆS-HANSEN J, KRISTENSEN GH, STROOMBERG HV, et al. Surgical approaches and outcomes in living donor nephrectomy: a systematic review and meta-analysis[J]. Eur Urol Focus, 2022, 8(6): 1795-1801. DOI: 10.1016/j.euf.2022.03.021. [7] CINTORINO D, PAGANO D, BONSIGNORE P, et al. Evolution of technique in laparoscopic donor nephrectomy: a single center experience[J]. J Laparoendosc Adv Surg Tech A, 2017, 27(7): 666-668. DOI: 10.1089/lap.2017.0140. [8] DAVIDIUK AJ, PARKER AS, THOMAS CS, et al. Mayo adhesive probability score: an accurate image-based scoring system to predict adherent perinephric fat in partial nephrectomy[J]. Eur Urol, 2014, 66(6): 1165-1171. DOI: 10.1016/j.eururo.2014.08.054. [9] SCHWARTZ FR, SHAW BI, LEREBOURS R, et al. Correlation of preoperative imaging characteristics with donor outcomes and operative difficulty in laparoscopic donor nephrectomy[J]. Am J Transplant, 2020, 20(3): 752-760. DOI: 10.1111/ajt.15608. [10] RAMAN JD, REYNOLDS C, HANNON M. An increasing proportion of perinephric to subcutaneous fat is associated with adverse perioperative outcomes of robotic partial nephrectomy[J]. J Robot Surg, 2016, 10(3): 255-259. DOI: 10.1007/s11701-016-0593-9. [11] CLAVIEN PA, BARKUN J, DE OLIVEIRA ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience[J]. Ann Surg, 2009, 250(2): 187-196. DOI: 10.1097/SLA.0b013e3181b13ca2. [12] GROSSO AA, SESSA F, CAMPI R, et al. Intraoperative and postoperative surgical complications after ureteroscopy, retrograde intrarenal surgery, and percutaneous nephrolithotomy: a systematic review[J]. Minerva Urol Nephrol, 2021, 73(3): 309-332. DOI: 10.23736/S2724-6051.21.04294-4. [13] KONAN A, PITON G, RONOT M, et al. Abdominal atherosclerosis is not a risk factor of nonocclusive mesenteric ischemia among critically ill patients: a propensity matching study[J]. Ann Intensive Care, 2022, 12(1): 117. DOI: 10.1186/s13613-022-01096-4. [14] AGATSTON AS, JANOWITZ WR, HILDNER FJ, et al. Quantification of coronary artery calcium using ultrafast computed tomography[J]. J Am Coll Cardiol, 1990, 15(4): 827-832. DOI: 10.1016/0735-1097(90)90282-t. [15] ELMARAEZY A, ABUSHOUK AI, KAMEL M, et al. Should hand-assisted retroperitoneoscopic nephrectomy replace the standard laparoscopic technique for living donor nephrectomy? a meta-analysis[J]. Int J Surg, 2017, 40: 83-90. DOI: 10.1016/j.ijsu.2017.02.018. [16] TABATABAI S, DO Q, MIN J, et al. Obesity and perioperative outcomes in older surgical patients undergoing elective spine and major arthroplasty surgery[J]. J Clin Anesth, 2021, 75: 110475. DOI: 10.1016/j.jclinane.2021.110475. [17] KANO T, KIM H, KAWAKAMI M, et al. Preoperative factors affecting the operative outcomes of laparoscopic nephrectomy[J]. Int J Urol, 2022, 29(7): 757-763. DOI: 10.1111/iju.14892. [18] KAZAURE HS, ROMAN SA, SOSA JA. Obesity is a predictor of morbidity in 1, 629 patients who underwent adrenalectomy[J]. World J Surg, 2011, 35(6): 1287-1295. DOI: 10.1007/s00268-011-1070-2. [19] LINDNER U, LAWRENTSCHUK N, ABOUASSALY R, et al. Radical prostatectomy in obese patients: improved surgical outcomes in recent years[J]. Int J Urol, 2010, 17(8): 727-732. DOI: 10.1111/j.1442-2042.2010.02570.x. [20] ONG CSH, LAW TYX, MOK A, et al. The impact of body mass index on oncological and surgical outcomes of patients undergoing nephrectomy: a systematic review and meta-analysis[J]. BJU Int, 2023, 132(6): 608-618. DOI: 10.1111/bju.16103. [21] MAURITS JSF, SEDELAAR JPM, ABEN KKH, et al. The association of body composition with postoperative complications and length of hospital stay after radical or partial nephrectomy in patients with renal cell cancer: a multicenter population-based cohort study[J]. Transl Androl Urol, 2022, 1(12): 1667-1679. DOI: 10.21037/tau-22-367. [22] TAKAGI K, KIMENAI HJAN, TERKIVATAN T, et al. A novel difficulty grading system for laparoscopic living donor nephrectomy[J]. Surg Endosc, 2021, 35(6): 2889-2895. DOI: 10.1007/s00464-020-07727-w. [23] KUMAZAWA T, TSUCHIYA N, INOUE T, et al. Association between various indices of obesity and intraoperative factors in laparoscopic donor nephrectomy[J]. J Laparoendosc Adv Surg Tech A, 2012, 22(6): 567-571. DOI: 10.1089/lap.2011.0472. [24] YAO Y, XU Y, GU L, et al. The Mayo adhesive probability score predicts longer dissection time during laparoscopic partial nephrectomy[J]. J Endourol, 2020, 34(5): 594-599. DOI: 10.1089/end.2019.0687. [25] DARIANE C, LE GUILCHET T, HUREL S, et al. Prospective assessment and histological analysis of adherent perinephric fat in partial nephrectomies[J]. Urol Oncol, 2017, 35(2): 39. e9-39. e17. DOI: 10.1016/j.urolonc.2016.09.008. [26] YUAN Y, FENG H, KANG Z, et al. Mayo adhesive probability score is associated with perioperative outcomes in retroperitoneal laparoscopic adrenalectomy[J]. ANZ J Surg, 2022, 92(12): 3273-3277. DOI: 10.1111/ans.17983. [27] FANG L, LI H, ZHANG T, et al. Analysis of predictors of adherent perinephric fat and its impact on perioperative outcomes in laparoscopic partial nephrectomy: a retrospective case-control study[J]. World J Surg Oncol, 2021, 19(1): 319. DOI: 10.1186/s12957-021-02429-6. [28] COCKERILL KJ, YOUNG S, T BALL C, et al. The association of the Mayo adhesive probability (MAP) score with total operative time in patients undergoing hand-assisted laparoscopic donor nephrectomy[J]. Urology, 2019, 124: 142-147. DOI: 10.1016/j.urology.2018.10.041. [29] LUZZAGO S, PALUMBO C, ROSIELLO G, et al. Metabolic syndrome predicts worse perioperative outcomes in patients treated with partial nephrectomy for renal cell carcinoma[J]. Urology, 2020, 140: 91-97. DOI: 10.1016/j.urology.2020.02.019. [30] SHARIQ OA, FRUTH KM, HANSON KT, et al. Metabolic syndrome is associated with increased postoperative complications and use of hospital resources in patients undergoing laparoscopic adrenalectomy[J]. Surgery, 2018, 163(1): 167-175. DOI: 10.1016/j.surg.2017.06.023. [31] DI MAIDA F, VITTORI G, CAMPI R, et al. Clinical predictors and significance of adherent perinephric fat assessed with Mayo adhesive probability (MAP) score and perinephric fat surface density (PnFSD) at the time of partial nephrectomy for localized renal mass. a single high-volume referral center experience[J]. Minerva Urol Nephrol, 2021, 73(2): 225-232. DOI: 10.23736/S2724-6051.20.03698-X. [32] PORPIGLIA F, RENARD J, BILLIA M, et al. Is renal warm ischemia over 30 minutes during laparoscopic partial nephrectomy possible? one-year results of a prospective study[J]. Eur Urol, 2007, 52(4): 1170-1178. DOI: 10.1016/j.eururo.2007.04.024. [33] GÜNAYDIN B, UÇAR T, ARPALI E, et al. Hand-assisted laparoscopic donor nephrectomy: 1864 cases in 15 years of experience[J]. Turk J Med Sci, 2022, 52(4): 1322-1328. DOI: 10.55730/1300-0144.5438. [34] KOK NF, DOLS LF, HUNINK MG, et al. Complex vascular anatomy in live kidney donation: imaging and consequences for clinical outcome[J]. Transplantation, 2008, 85(12): 1760-1765. DOI: 10.1097/TP.0b013e318172802d. [35] KAWAKATSU S, YAMAGUCHI J, MIZUNO T, et al. Early prediction of a serious postoperative course in perihilar cholangiocarcinoma: trajectory analysis of the comprehensive complication index[J]. Ann Surg, 2023, 277(3): 475-483. DOI: 10.1097/SLA.0000000000005162. [36] GIULIANI T, DE PASTENA M, PAIELLA S, et al. Pancreatic enucleation patients share the same quality of life as the general population at long-term follow-up: a propensity score-matched analysis[J]. Ann Surg, 2023, 277(3): e609-e616. DOI: 10.1097/SLA.0000000000004911. [37] KENGSAKUL M, NIEUWENHUYZEN-DE BOER GM, UDOMKARNJANANUN S, et al. Clinical validation and comparison of the comprehensive complication index and Clavien-Dindo classification in predicting post-operative outcomes after cytoreductive surgery in advanced ovarian cancer[J]. Int J Gynecol Cancer, 2023, 33(2): 263-270. DOI: 10.1136/ijgc-2022-003998. [38] METZEMAEKERS J, BOUWMAN L, DE VOS M, et al. Clavien-Dindo, comprehensive complication index and classification of intraoperative adverse events: a uniform and holistic approach in adverse event registration for (deep) endometriosis surgery[J]. Hum Reprod Open, 2023(2): hoad019. DOI: 10.1093/hropen/hoad019. -





 下载:
下载: