Influencing factors of survival of patients with airway stenosis requiring clinical interventions after lung transplantation
-
摘要:
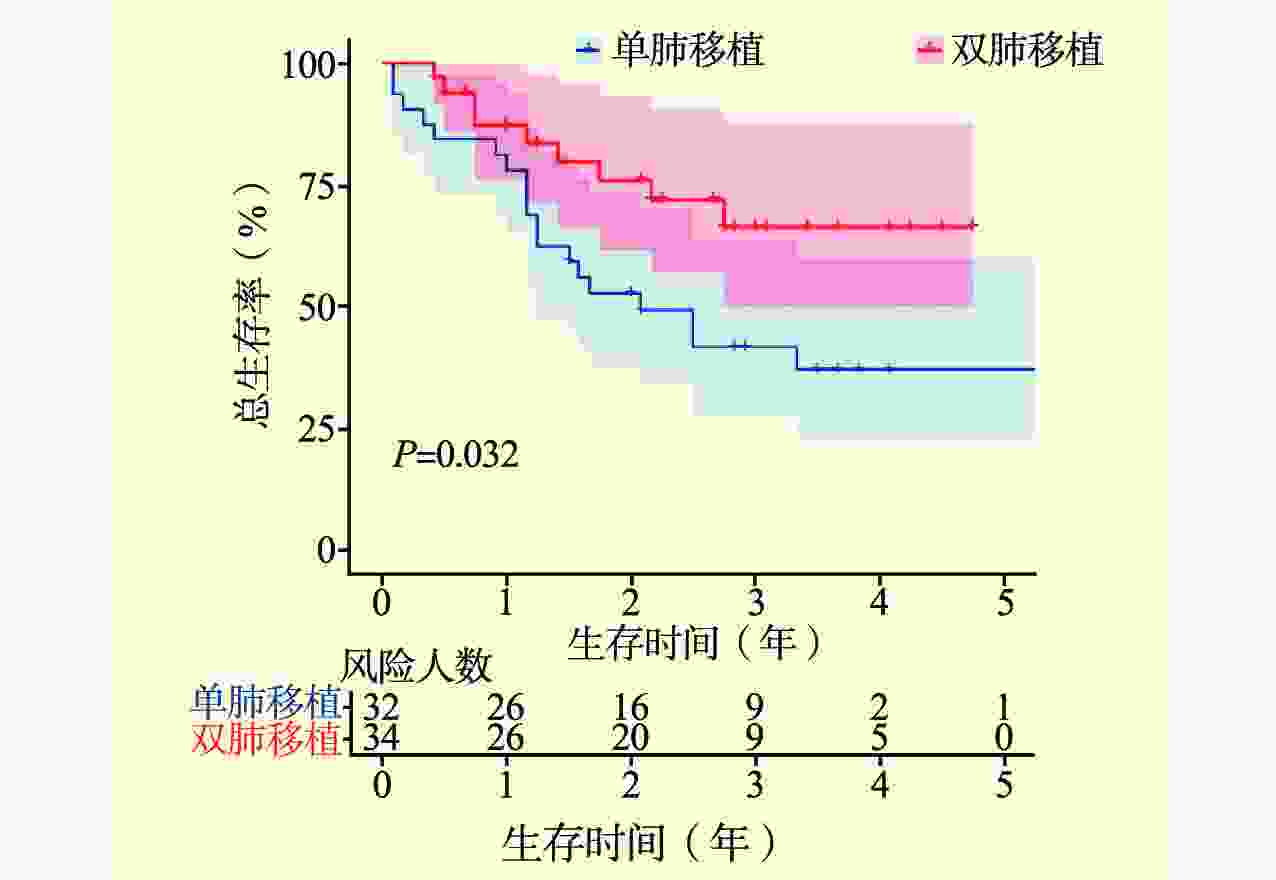
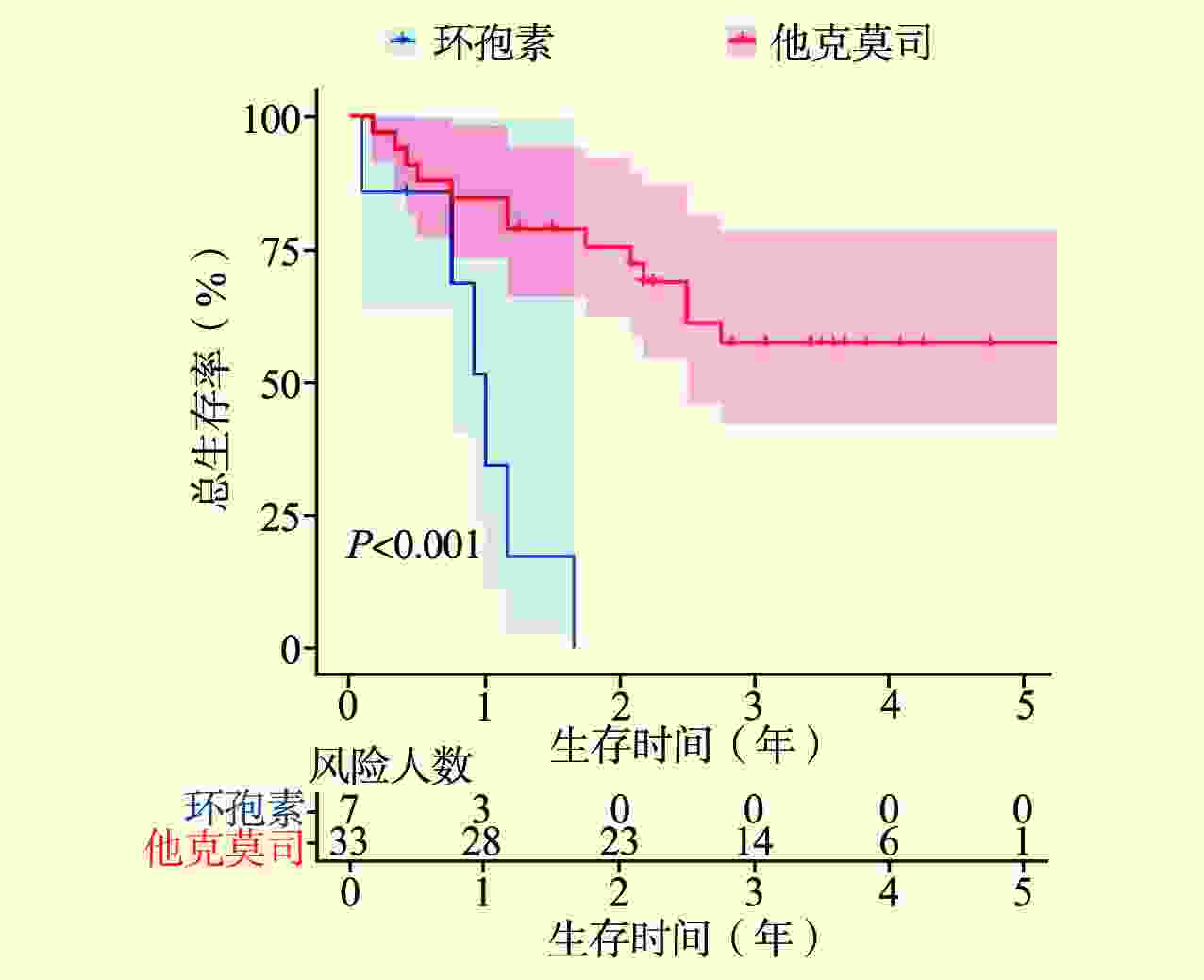
目的 分析肺移植术后需要临床干预的气道狭窄患者生存结局的影响因素。 方法 回顾性分析肺移植术后需要临床干预的66例气道狭窄患者的临床资料。采用单因素和多因素Cox回归模型分析所有气道狭窄患者和早期气道狭窄患者生存结局的影响因素,采用Kaplan-Meier法计算总生存率并绘制生存曲线。 结果 66例气道狭窄患者,中位无气道狭窄时间为72(52,102)d,27%(18/66)发生中心气道狭窄,73%(48/66)发生远端气道狭窄。术后机械通气时间[风险比(HR)1.037,95%可信区间(CI)1.005~1.070,P=0.024]和手术类型(HR 0.400,95% CI 0.177~0.903,P=0.027)均与肺移植术后气道狭窄患者的生存结局存在相关性,术后机械通气时间越长,受者死亡风险越高;接受双肺移植的气道狭窄患者的总生存率优于单肺移植。在亚组分析中,3级原发性移植物失功(PGD)(HR 4.577,95% CI 1.439~14.555,P=0.010)和免疫抑制药(HR 0.079,95% CI 0.022~0.287,P<0.001)与肺移植术后早期气道狭窄患者生存结局均存在相关性;无3级PGD的肺移植术后早期气道狭窄患者的总生存率优于有3级PGD的患者,使用他克莫司的肺移植术后早期气道狭窄患者的总生存率优于使用环孢素的患者。 结论 术后机械通气时间长、单肺移植手术方式、3级PGD和使用环孢素可能影响肺移植术后气道狭窄患者的生存。 Abstract:Objective To analyze the influencing factors of survival of patients with airway stenosis requiring clinical interventions after lung transplantation. Methods Clinical data of 66 patients with airway stenosis requiring clinical interventions after lung transplantation were retrospectively analyzed. Univariate and multivariate Cox’s regression models were adopted to analyze the influencing factors of survival of all patients with airway stenosis and those with early airway stenosis. Kaplan-Meier method was used to calculate the overall survival and delineate the survival curve. Results For 66 patients with airway stenosis, the median airway stenosis-free time was 72 (52,102) d, 27% (18/66) for central airway stenosis and 73% (48/66) for distal airway stenosis. Postoperative mechanical ventilation time [hazard ratio (HR) 1.037, 95% confidence interval (CI) 1.005-1.070, P=0.024] and type of surgery (HR 0.400, 95%CI 0.177-0.903, P=0.027) were correlated with the survival of patients with airway stenosis after lung transplantation. The longer the postoperative mechanical ventilation time, the higher the risk of mortality of the recipients. The overall survival of airway stenosis recipients undergoing bilateral lung transplantation was better than that of their counterparts after single lung transplantation. Subgroup analysis showed that grade 3 primary graft dysfunction (PGD) (HR 4.577, 95%CI 1.439-14.555, P=0.010) and immunosuppressive drugs (HR 0.079, 95%CI 0.022-0.287, P<0.001) were associated with the survival of patients with early airway stenosis after lung transplantation. The overall survival of patients with early airway stenosis after lung transplantation without grade 3 PGD was better compared with that of those with grade 3 PGD. The overall survival of patients with early airway stenosis after lung transplantation treated with tacrolimus was superior to that of their counterparts treated with cyclosporine. Conclusions Long postoperative mechanical ventilation time, single lung transplantation, grade 3 PGD and use of cyclosporine may affect the survival of patients with airway stenosis after lung transplantation. -
表 1 肺移植术后气道狭窄患者生存结局的单因素和多因素分析
Table 1. Univariate and multivariate analysis of survival outcomes in patients with airway stenosis after lung transplantation
变量 气道狭窄患者(n=66) 单因素分析 多因素分析 HR(95%CI) P值 HR(95%CI) P值 性别[n(%)] 男 54(82) 参照值 女 12(18) 1.513(0.571~4.009) 0.405 年龄[M(P25,P75),岁] 55(48,61) 1.028(0.992~1.065) 0.131 BMI($\bar x $±s,kg/m2) 20±4 1.070(0.976~1.172) 0.149 供者末次氧合指数[M(P25,P75),mmHg①] 435(390,466) 1.004(0.998~1.010) 0.192 冷缺血时间[M(P25,P75),h] 7.1(5.6,8.1) 0.916(0.755~1.111) 0.373 手术类型[n(%)] 0.400(0.177~0.903) 0.027 单肺移植 32(48) 参照值 双肺移植 34(52) 0.433(0.196~0.959) 0.039 手术时间[M(P25,P75),h] 5.7(4.4,6.7) 0.917(0.745~1.128) 0.412 ECMO使用[n(%)] 43(65) 0.953(0.439~2.066) 0.902 术后机械通气时间[M(P25,P75),d] 2.0(1.0,2.8) 1.030(1.000~1.061) 0.050 1.037(1.005~1.070) 0.024 术后ICU入住时间[M(P25,P75),d] 5(3,6) 0.998(0.960~1.038) 0.920 无气道狭窄时间[M(P25,P75),d] 72(52,102) 0.999(0.991~1.008) 0.875 狭窄位置[n(%)] 中心气道狭窄 18(27) 参照值 远端气道狭窄 48(73) 0.793(0.358~1.755) 0.567 术后FEV1/FVC[M(P25,P75),%] 80(69,91) 1.704(0.385~7.541) 0.482 术后6MWT[M(P25,P75),m] 450(335,538) 1.001(0.997~1.004) 0.756 3级PGD[n(%)] 11(17) 1.824(0.774~4.301) 0.170 免疫抑制药[n(%)] 环孢素 12(18) 参照值 他克莫司 54(82) 0.517(0.219~1.222) 0.133 注:①1 mmHg=0.133kPa。 表 2 肺移植术后早期气道狭窄患者生存结局的单因素和多因素分析
Table 2. Univariate and multivariate analysis of survival outcomes in patients with early airway stenosis after lung transplantation
变量 早期气道狭窄患者
(n=40)单因素分析 多因素分析 HR(95%CI) P值 HR(95%CI) P值 性别[n(%)] 男 32(80) 参照值 女 8(20) 1.642(0.536~5.031) 0.385 年龄[M(P25,P75),岁] 54(44,61) 1.015(0.972~1.059) 0.495 BMI($\bar x $±s,kg/m2) 20±8 1.081(0.978~1.194) 0.127 供者末次氧合指数
[M(P25,P75),mmHg①]449(403,473) 1.003(0.995~1.010) 0.464 冷缺血时间[M(P25,P75),h] 8.0(6.8,9.0) 0.876(0.678~1.133) 0.314 手术类型[n(%)] 单肺移植 19(48) 参照值 双肺移植 21(52) 0.621(0.249~1.545) 0.306 手术时间[M(P25,P75),h] 5.7(4.5,6.8) 0.929(0.747~1.154) 0.505 ECMO使用[n(%)] 28(70) 0.879(0.334~2.315) 0.794 术后机械通气时间
[M(P25,P75),d]2(1,3) 1.028(0.998~1.060) 0.068 1.023(0.988~1.058) 0.198 术后ICU入住时间[M(P25,P75),d] 5(3,6) 1.003(0.966~1.040) 0.888 无气道狭窄时间[M(P25,P75),d] 55(45,69) 0.997(0.973~1.022) 0.828 狭窄位置[n(%)] 中心气道狭窄 9(22) 参照值 远端气道狭窄 31(78) 0.589(0.224~1.551) 0.284 术后FEV1/FVC[M(P25,P75),%] 81(69,91) 0.946(0.183~4.885) 0.947 术后6MWT[M(P25,P75),m] 482(360,542) 0.999(0.996~1.003) 0.663 3级PGD[n(%)] 7(18) 2.707(1.020~7.180) 0.045 4.577(1.439~14.555) 0.010 免疫抑制药[n(%)] 0.079(0.022~0.287) <0.001 环孢素 7(17) 参照值 他克莫司 33(83) 0.147(0.048~0.451) 0.001 注:①1 mmHg=0.133kPa。 -
[1] HUANG H, YAN HJ, ZHENG XY, et al. Right lung transplantation with a left-to-right inverted anastomosis in a rat model[J]. JTCVS Open, 2022, 10: 429-439. DOI: 10.1016/j.xjon.2022.01.020. [2] 王红梅, 吴波, 范立, 等. 肺移植治疗终末期肺动脉高压的预后分析[J]. 中国呼吸与危重监护杂志, 2022, 21(8): 572-576.WANG HM, WU B, FAN L, et al. Prognosis of lung transplantation in the treatment of end-stage pulmonary arterial hypertension[J]. Chin J Respir Crit Care Med, 2022, 21(8): 572-576. [3] HANNA K, CALVELLI H, KASHEM MA, et al. Donor and recipient age in interstitial lung disease: types of lung transplant survival outcomes[J]. J Surg Res, 2024, 293: 136-143. DOI: 10.1016/j.jss.2023.07.012. [4] MEI B, LI X, WENG J, et al. Donor and recipient age matching in lung transplantation: a retrospective study[J]. Heliyon, 2023, 9(12): e22753. DOI: 10.1016/j.heliyon.2023.e22753. [5] VALAPOUR M, LEHR CJ, SCHLADT DP, et al. OPTN/SRTR 2021 annual data report: lung[J]. Am J Transplant, 2023, 23(2 Suppl 1): S379-S442. DOI: 10.1016/j.ajt.2023.02.009. [6] ZHOU Y, QIN Z, WANG G, et al. Current status and training needs of trainee anesthesiologists in lung transplantation anesthesia in China: a single-center survey[J]. Heliyon, 2022, 8(12): e12428. DOI: 10.1016/j.heliyon.2022.e12428. [7] JINDAL A, AVASARAL S, GREWAL H, et al. Airway complications following lung transplantation[J]. Indian J Thorac Cardiovasc Surg, 2022, 38(Suppl 2): 326-334. DOI: 10.1007/s12055-022-01376-5. [8] VAN PEL R, GAN CT, VAN DER BIJ W, et al. Three decades single center experience of airway complications after lung transplantation[J]. Transpl Int, 2023, 36: 11519. DOI: 10.3389/ti.2023.11519. [9] KRAFT BD, MAHMOOD K, HARLAN NP, et al. Hyperbaric oxygen therapy to prevent central airway stenosis after lung transplantation[J]. J Heart Lung Transplant, 2021, 40(4): 269-278. DOI: 10.1016/j.healun.2021.01.008. [10] 杨航, 卫栋, 张稷, 等. 肺移植术后中心气道狭窄危险因素分析[J]. 器官移植, 2022, 13(2): 240-245. DOI: 10.3969/j.issn.1674-7445.2022.02.013.YANG H, WEI D, ZHANG J, et al. Risk factors analysis of central airway stenosis after lung transplantation[J]. Organ Transplant, 2022, 13(2): 240-245. DOI: 10.3969/j.issn.1674-7445.2022.02.013. [11] MARTINOD E, DUTAU H, GUIBERT N. Management of airway complications after lung transplantation: is there an ideal stent?[J]. J Thorac Dis, 2022, 14(9): 3111-3115. DOI: 10.21037/jtd-22-858. [12] SANTACRUZ JF, MEHTA AC. Airway complications and management after lung transplantation: ischemia, dehiscence, and stenosis[J]. Proc Am Thorac Soc, 2009, 6(1): 79-93. DOI: 10.1513/pats.200808-094GO. [13] HUANG J, LIN J, ZHENG Z, et al. Risk factors and prognosis of airway complications in lung transplant recipients: a systematic review and meta-analysis[J]. J Heart Lung Transplant, 2023, 42(9): 1251-1260. DOI: 10.1016/j.healun.2023.04.011. [14] CRESPO MM, MCCARTHY DP, HOPKINS PM, et al. ISHLT consensus statement on adult and pediatric airway complications after lung transplantation: definitions, grading system, and therapeutics[J]. J Heart Lung Transplant, 2018, 37(5): 548-563. DOI: 10.1016/j.healun.2018.01.1309. [15] MOHANKA M, BANGA A. Alterations in pulmonary physiology with lung transplantation[J]. Compr Physiol, 2023, 13(1): 4269-4293. DOI: 10.1002/cphy.c220008. [16] MORENO P, ALVAREZ A, ALGAR FJ, et al. Incidence, management and clinical outcomes of patients with airway complications following lung transplantation[J]. Eur J Cardiothorac Surg, 2008, 34(6): 1198-1205. DOI: 10.1016/j.ejcts.2008.08.006. [17] KIM HH, JO KW, SHIM TS, et al. Incidence, risk factors, and clinical characteristics of airway complications after lung transplantation[J]. Sci Rep, 2023, 13(1): 667. DOI: 10.1038/s41598-023-27864-1. [18] CRESPO MM. Airway complications in lung transplantation[J]. J Thorac Dis, 2021, 13(11): 6717-6724. DOI: 10.21037/jtd-20-2696. [19] ARYAL S, NATHAN SD. Single vs. bilateral lung transplantation: when and why[J]. Curr Opin Organ Transplant, 2018, 23(3): 316-323. DOI: 10.1097/MOT.0000000000000527. [20] SUBRAMANIAN M, MEYERS BF. Lung transplant procedure of choice: bilateral transplantation versus single transplantation complications, quality of life, and survival[J]. Clin Chest Med, 2023, 44(1): 47-57. DOI: 10.1016/j.ccm.2022.10.003. [21] WILSON-SMITH AR, KIM YS, EVANS GE, et al. Single versus double lung transplantation for fibrotic disease-systematic review[J]. Ann Cardiothorac Surg, 2020, 9(1): 10-19. DOI: 10.21037/acs.2019.12.04. [22] RUTTMANN E, ULMER H, MARCHESE M, et al. Evaluation of factors damaging the bronchial wall in lung transplantation[J]. J Heart Lung Transplant, 2005, 24(3): 275-281. DOI: 10.1016/j.healun.2004.01.008. [23] SUBASI M, DUGER M. Preoperative risk factors of airway complications in adult lung transplant recipients: a systematic review and meta-analysis[J]. Turk Gogus Kalp Damar Cerrahisi Derg, 2023, 31(4): 517-529. DOI: 10.5606/tgkdc.dergisi.2023.25399. [24] SCHWER CI, ROTH T, GASS M, et al. Risk factors for prolonged mechanical ventilation and delayed extubation following bimaxillary orthognathic surgery: a single-center retrospective cohort study[J]. J Clin Med, 2022, 11(13): 3829. DOI: 10.3390/jcm11133829. [25] HADEM J, GOTTLIEB J, SEIFERT D, et al. Prolonged mechanical ventilation after lung transplantation-a single-center study[J]. Am J Transplant, 2016, 16(5): 1579-1587. DOI: 10.1111/ajt.13632. [26] 张静, 王卓, 邓宇, 等. 肺移植后原发性移植物功能障碍的研究进展[J]. 武汉大学学报(医学版), 2021, 42(4): 564-569. DOI: 10.14188/j.1671-8852.2021.0020.ZHANG J, WANG Z, DENG Y, et al. Research progress of primary graft dysfunction after lung transplantation[J]. Med J Wuhan Univ, 2021, 42(4): 564-569. DOI: 10.14188/j.1671-8852.2021.0020. [27] CANTU E, DIAMOND JM, CEVASCO M, et al. Contemporary trends in PGD incidence, outcomes, and therapies[J]. J Heart Lung Transplant, 2022, 41(12): 1839-1849. DOI: 10.1016/j.healun.2022.08.013. [28] MUNSHI L, CYPEL M, MOHAMED A, et al. The association between extravascular lung water and critical care outcomes following bilateral lung transplantation[J]. Transplant Direct, 2022, 8(10): e1376. DOI: 10.1097/TXD.0000000000001376. [29] HALPERN SE, AU S, KESSELI SJ, et al. Lung transplantation using allografts with more than 8 hours of ischemic time: a single-institution experience[J]. J Heart Lung Transplant, 2021, 40(11): 1463-1471. DOI: 10.1016/j.healun.2021.05.008. [30] DIAMOND JM, LEE JC, KAWUT SM, et al. Clinical risk factors for primary graft dysfunction after lung transplantation[J]. Am J Respir Crit Care Med, 2013, 187(5): 527-534. DOI: 10.1164/rccm.201210-1865OC. [31] WHITSON BA, NATH DS, JOHNSON AC, et al. Risk factors for primary graft dysfunction after lung transplantation[J]. J Thorac Cardiovasc Surg, 2006, 131(1): 73-80. DOI: 10.1016/j.jtcvs.2005.08.039. [32] HUNT ML, CANTU E. Primary graft dysfunction after lung transplantation[J]. Curr Opin Organ Transplant, 2023, 28(3): 180-186. DOI: 10.1097/MOT.0000000 000001065. [33] DELLGREN G, LUND TK, RAIVIO P, et al. Effect of once-per-day tacrolimus versus twice-per-day ciclosporin on 3-year incidence of chronic lung allograft dysfunction after lung transplantation in Scandinavia (ScanCLAD): a multicentre randomised controlled trial[J]. Lancet Respir Med, 2024, 12(1): 34-44. DOI: 10.1016/S2213-2600(23)00293-X. [34] PINSKER KL, VEITH FJ, KAMHOLZ SL, et al. Bronchial anastomotic healing in canine lung allotransplants treated with cyclosporine[J]. Transplantation, 1985, 40(2): 143-146. DOI: 10.1097/00007890-198508000-00006. [35] HIRAI T, WADA H, HASEGAWA S, et al. The immunosuppressive effect of FK 506 on canine lung transplantation[J]. J Thorac Cardiovasc Surg, 1992, 103(6): 1127-1135. DOI: 10.1016/S0022-5223(19)34877-9. [36] HACHEM RR, YUSEN RD, CHAKINALA MM, et al. A randomized controlled trial of tacrolimus versus cyclosporine after lung transplantation[J]. J Heart Lung Transplant, 2007, 26(10): 1012-1018. DOI: 10.1016/j.healun.2007.07.027. [37] TREEDE H, GLANVILLE AR, KLEPETKO W, et al. Tacrolimus and cyclosporine have differential effects on the risk of development of bronchiolitis obliterans syndrome: results of a prospective, randomized international trial in lung transplantation[J]. J Heart Lung Transplant, 2012, 31(8): 797-804. DOI: 10.1016/j.healun.2012.03.008. [38] SARAHRUDI K, ESTENNE M, CORRIS P, et al. International experience with conversion from cyclosporine to tacrolimus for acute and chronic lung allograft rejection[J]. J Thorac Cardiovasc Surg, 2004, 127(4): 1126-1132. DOI: 10.1016/j.jtcvs.2003.11.009. -




 下载:
下载: