| [1] |
FREE RJ, SAPIANO MRP, CHAVEZ ORTIZ JL, et al. Continued stabilization of blood collections and transfusions in the United States: findings from the 2021 National Blood Collection and Utilization Survey[J]. Transfusion, 2023, 63(Suppl 4): S8-S18. DOI: 10.1111/trf.17360.
|
| [2] |
JAHR JS. Blood substitutes: basic science, translational studies and clinical trials[J]. Front Med Technol, 2022, 4: 989829. DOI: 10.3389/fmedt.2022.989829.
|
| [3] |
CAO M, ZHAO Y, HE H, et al. New applications of HBOC-201: a 25-year review of the literature[J]. Front Med (Lausanne), 2021, 8: 794561. DOI: 10.3389/fmed.2021.794561.
|
| [4] |
刘嘉馨, 杨成民. 红细胞代用品研究进展与现状[J]. 中国输血杂志, 2022, 35(8): 785-790. DOI: 10.13303/j.cjbt.issn.1004-549x.2022.08.002.LIU JX, YANG CM. Research progress and future of red blood cell substitutes[J]. Chin J Blood Transfus, 2022, 35(8): 785-790. DOI: 10.13303/j.cjbt.issn.1004-549x.2022.08.002.
|
| [5] |
高菲, 王煜, 杜嘉祥, 等. 遗传修饰猪模型在生物医学及农业领域研究进展及应用[J]. 遗传, 2023, 45(1): 6-28. DOI: 10.16288/j.yczz.22-313.GAO F, WANG Y, DU JX, et al. Advances and applications of genetically modified pig models in biomedical and agricultural field[J]. Hereditas, 2023, 45(1): 6-28. DOI: 10.16288/j.yczz.22-313.
|
| [6] |
SMOOD B, HARA H, SCHOEL LJ, et al. Genetically-engineered pigs as sources for clinical red blood cell transfusion: what pathobiological barriers need to be overcome?[J]. Blood Rev, 2019, 35: 7-17. DOI: 10.1016/j.blre.2019.01.003.
|
| [7] |
RYCZEK N, HRYHOROWICZ M, ZEYLAND J, et al. CRISPR/Cas technology in pig-to-human xenotransplantation research[J]. Int J Mol Sci, 2021, 22(6): 3196. DOI: 10.3390/ijms22063196.
|
| [8] |
COOPER DKC. Introduction: the present status of xenotransplantation research[J]. Methods Mol Biol, 2020, 2110: 1-25. DOI: 10.1007/978-1-0716-0255-3_1.
|
| [9] |
EISENSON DL, HISADOME Y, YAMADA K. Progress in xenotransplantation: immunologic barriers, advances in gene editing, and successful tolerance induction strategies in pig-to-primate transplantation[J]. Front Immunol, 2022, 13: 899657. DOI: 10.3389/fimmu.2022.899657.
|
| [10] |
LEI T, CHEN L, WANG K, et al. Genetic engineering of pigs for xenotransplantation to overcome immune rejection and physiological incompatibilities: the first clinical steps[J]. Front Immunol, 2022, 13: 1031185. DOI: 10.3389/fimmu.2022.1031185.
|
| [11] |
YAMAMOTO T, BIKHET MH, MARQUES MB, et al. Initial experimental experience of triple-knockout pig red blood cells as potential sources for transfusion in alloimmunized patients with sickle cell disease[J]. Transfusion, 2021, 61(11): 3104-3118. DOI: 10.1111/trf.16667.
|
| [12] |
WANG ZY, BURLAK C, ESTRADA JL, et al. Erythrocytes from GGTA1/CMAH knockout pigs: implications for xenotransfusion and testing in non-human primates[J]. Xenotransplantation, 2014, 21(4): 376-384. DOI: 10.1111/xen.12106.
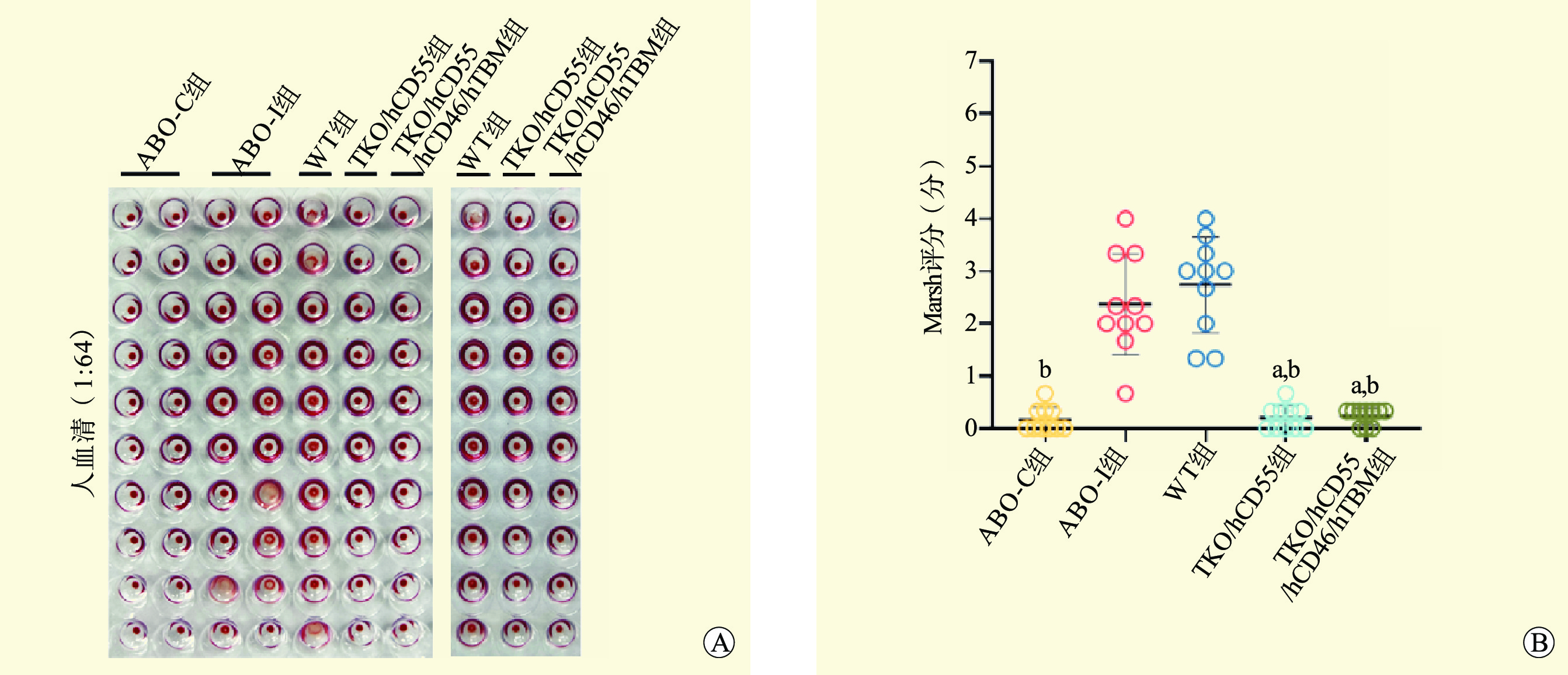
|
| [13] |
ABE T, KOMORI A, SHIRAISHI A, et al. Trauma complications and in-hospital mortality: failure-to-rescue[J]. Crit Care, 2020, 24(1): 223. DOI: 10.1186/s13054-020-02951-1.
|
| [14] |
SZYMANSKI L, GOŁASZEWSKA K, MAŁKOWSKA J, et al. Safety and performance of hemostatic powders[J]. Med Devices (Auckl), 2023, 16: 133-144. DOI: 10.2147/MDER.S407838.
|
| [15] |
MCCOY CC, BRENNER M, DUCHESNE J, et al. Back to the future: whole blood resuscitation of the severely injured trauma patient[J]. Shock, 2021, 56(1S): 9-15. DOI: 10.1097/SHK.0000000000001685.
|
| [16] |
HESLING JD, PAULSON MW, MCKAY JT, et al. Characterizing pediatric supermassive transfusion and the contributing injury patterns in the combat environment[J]. Am J Emerg Med, 2022, 51: 139-143. DOI: 10.1016/j.ajem.2021.10.032.
|
| [17] |
NARAYANAN D, HOGAN NB, SCHASER KA, et al. A case study in process improvement to minimize delays from obtaining blood for red cell exchange for a patient with sickle cell disease and multiple red blood cell alloantibodies[J]. Case Rep Hematol, 2022: 1562921. DOI: 10.1155/2022/1562921.
|
| [18] |
ROLLINS MR, CHOU ST. Adverse events of red blood cell transfusions in patients with sickle cell disease[J]. Transfus Apher Sci, 2022, 61(5): 103557. DOI: 10.1016/j.transci.2022.103557.
|
| [19] |
刘海艇, 谢秀巧, 郭永建, 等. 立即行动充分发挥患者血液管理在疾病大流行期间的重要基础作用——国际患者血液管理基金会和血液管理促进学会紧急呼吁[J]. 中国输血杂志, 2020, 33(6): 543-547. DOI: 10.13303/j.cjbt.issn.1004-549x.2020.06.001.LIU HT, XIE XQ, GUO YJ, et al. Take immediate action to fully leverage the important foundational role of patient blood management during the pandemic - urgent appeal from the International Patient Blood Management Foundation and the Society for the Promotion of Blood Management[J]. Chin J Blood Transfus, 2020, 33(6): 543-547. DOI: 10.13303/j.cjbt.issn.1004-549x.2020.06.001.
|
| [20] |
HOZAIN AE, O'NEILL JD, PINEZICH MR, et al. Xenogeneic cross-circulation for extracorporeal recovery of injured human lungs[J]. Nat Med, 2020, 26(7): 1102-1113. DOI: 10.1038/s41591-020-0971-8.
|
| [21] |
ROUHANI FJ, DOR FJ, COOPER DK. Investigation of red blood cells from alpha1, 3-galactosyltransferase-knockout pigs for human blood transfusion[J]. Transfusion, 2004, 44(7): 1004-1012. DOI: 10.1111/j.1537-2995.2004.04002.x.
|
| [22] |
LONG C, HARA H, PAWLIKOWSKI Z, et al. Genetically engineered pig red blood cells for clinical transfusion: initial in vitro studies[J]. Transfusion, 2009, 49(11): 2418-2429. DOI: 10.1111/j.1537-2995.2009.02306.x.
|
| [23] |
COOPER DKC, PIERSON RN 3RD. Milestones on the path to clinical pig organ xenotransplantation[J]. Am J Transplant, 2023, 23(3): 326-335. DOI: 10.1016/j.ajt.2022.12.023.
|
| [24] |
LEE H, PARK EM, KO N, et al. Effect of factor H on complement alternative pathway activation in human serum remains on porcine cells lacking N-glycolylneuraminic acid[J]. Front Immunol, 2022, 13: 859261. DOI: 10.3389/fimmu.2022.859261.
|
| [25] |
YAMAMOTO T, HARA H, AYARES D, et al. The problem of the "4th xenoantigen" after pig organ transplantation in non-human primates may be overcome by expression of human "protective" proteins[J]. Xenotransplantation, 2021, 28(2): e12658. DOI: 10.1111/xen.12658.
|
| [26] |
李丹妮, 赵艳双, 王轶, 等. 异种移植新进展: 从实验到临床[J]. 中国普外基础与临床杂志, 2022, 29(6): 705-710.LI DN, ZHAO YS, WANG Y, et al. New advances in xenotransplantation: from bench to bedside[J]. Chin J Base Clin Gen Surg, 2022, 29(6): 705-710.
|
| [27] |
CHRISTIANSEN D, MILLAND J, THORLEY BR, et al. A functional analysis of recombinant soluble CD46 in vivo and a comparison with recombinant soluble forms of CD55 and CD35 in vitro[J]. Eur J Immunol, 1996, 26(3): 578-585. DOI: 10.1002/eji.1830260312.
|
| [28] |
HARA H, LONG C, LIN YJ, et al. In vitro investigation of pig cells for resistance to human antibody-mediated rejection[J]. Transpl Int, 2008, 21(12): 1163-1174. DOI: 10.1111/j.1432-2277.2008.00736.x.
|
| [29] |
DERNSTEDT A, LEIDIG J, HOLM A, et al. Regulation of decay accelerating factor primes human germinal center B cells for phagocytosis[J]. Front Immunol, 2021, 11: 599647. DOI: 10.3389/fimmu.2020.599647.
|
| [30] |
CHABAN R, COOPER DKC, PIERSON RN 3RD. Pig heart and lung xenotransplantation: present status[J]. J Heart Lung Transplant, 2022, 41(8): 1014-1022. DOI: 10.1016/j.healun.2022.04.010.
|
| [31] |
周明, 邓阳阳, 戴一凡, 等. 猪肺异种移植的研究进展与发展方向[J]. 器官移植, 2017, 8(6): 476-479. DOI: 10.3969/j.issn.1674-7445.2017.06.013.ZHOU M, DENG YY, DAI YF, et al. Research progress and development direction of pig lung xenotransplantation[J]. Organ Transplant, 2017, 8(6): 476-479. DOI: 10.3969/j.issn.1674-7445.2017.06.013.
|
| [32] |
LI T, FENG H, DU J, et al. Serum antibody binding and cytotoxicity to pig cells in Chinese subjects: relevance to clinical renal xenotransplantation[J]. Front Immunol, 2022, 13: 844632. DOI: 10.3389/fimmu.2022.844632.
|
| [33] |
LIN CC, COOPER DK, DORLING A. Coagulation dysregulation as a barrier to xenotransplantation in the primate[J]. Transpl Immunol, 2009, 21(2): 75-80. DOI: 10.1016/j.trim.2008.10.008.
|
| [34] |
KIM H, HURH S, LEE SK, et al. Additive expression of hTBM on hCD46 stable cell line has synergistic effect on complement regulation[J]. Transplantation, 2018, 102: S743. DOI: 10.1097/01.tp.0000543735.57229.de.
|
| [35] |
PARK S, LEE H, PARK EM, et al. Initial investigation on the feasibility of porcine red blood cells from genetically modified pigs as an alternative to human red blood cells for transfusion[J]. Front Immunol, 2023, 14: 1298035. DOI: 10.3389/fimmu.2023.1298035.
|
| [36] |
于佳庆, 方一晽, 方铭慧, 等. 猪肾脏异种移植的研究进展[J]. 吉林大学学报(医学版), 2021, 47(3): 788-795. DOI: 10.13481/j.1671-587X.20210332.YU JQ, FANG YL, FANG MH, et al. Research progress in pig kidney xenotransplantation[J]. J Jilin Univ (Med Edit), 2021, 47(3): 788-795. DOI: 10.13481/j.1671-587X.20210332.
|
| [37] |
LASSITER G, OTSUKA R, HIROSE T, et al. TNX-1500, a crystallizable fragment-modified anti-CD154 antibody, prolongs nonhuman primate renal allograft survival[J]. Am J Transplant, 2023, 23(8): 1171-1181. DOI: 10.1016/j.ajt.2023.03.022.
|
| [38] |
COOPER DKC. The long and winding road to clinical xenotransplantation: a personal journey[J]. Eur Surg Res, 2022, 63(4): 165-172. DOI: 10.1159/000525757.
|





 下载:
下载: