Adenine phosphoribosyltransferase deficiency after kidney transplantation: a case report and literature review
-
摘要:
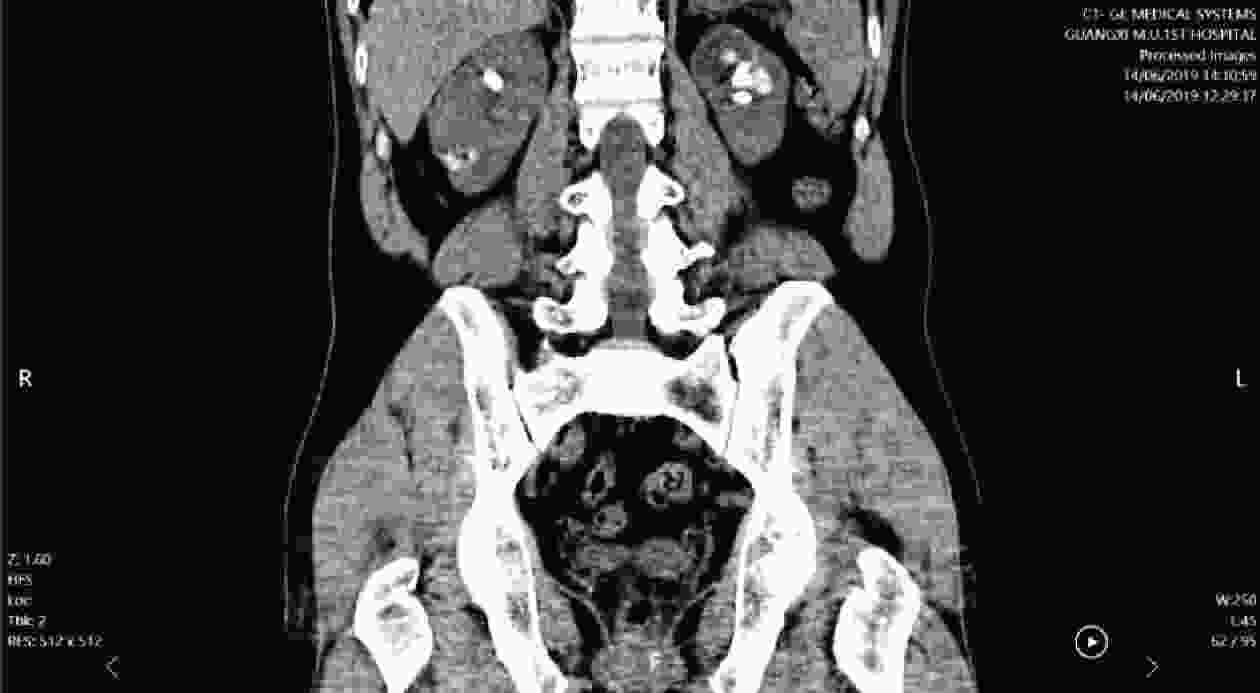
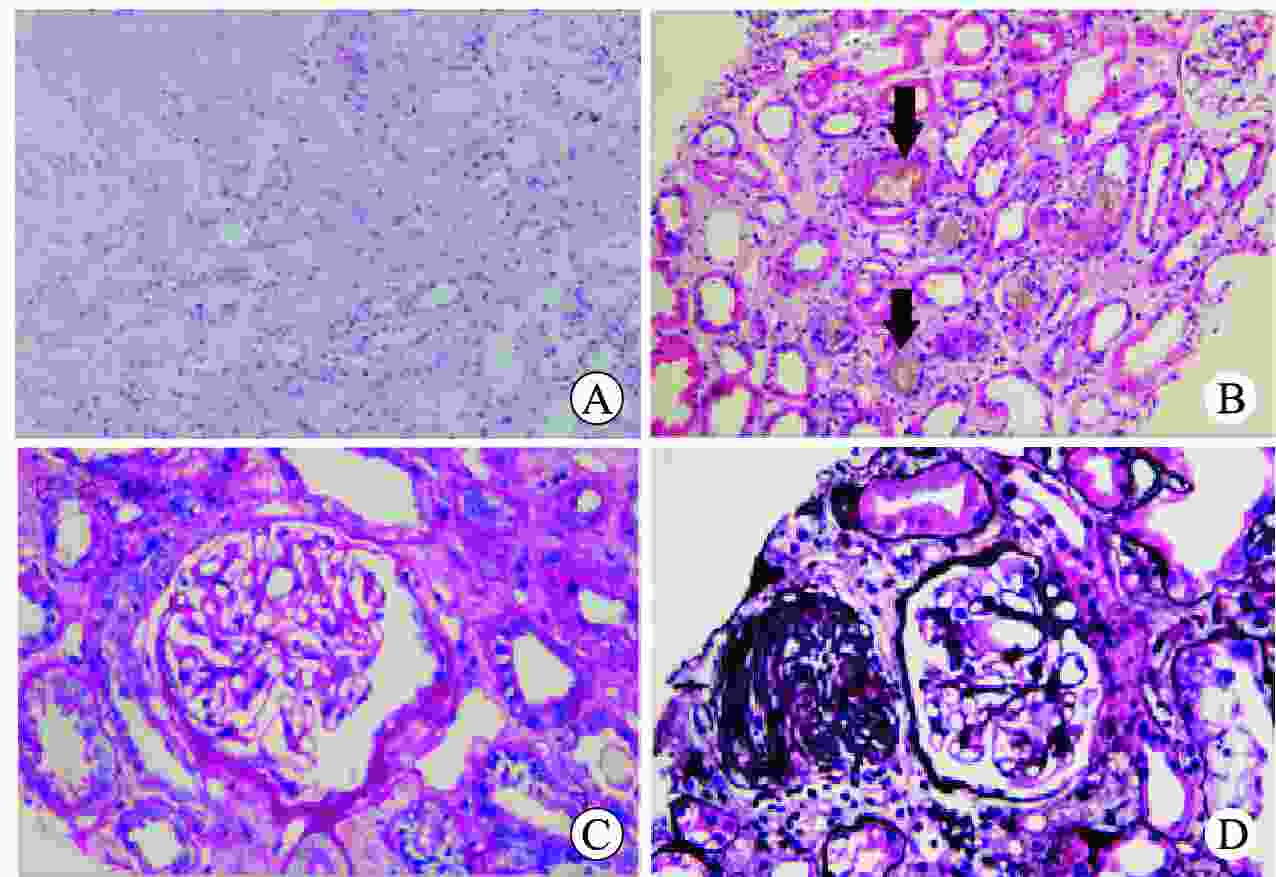
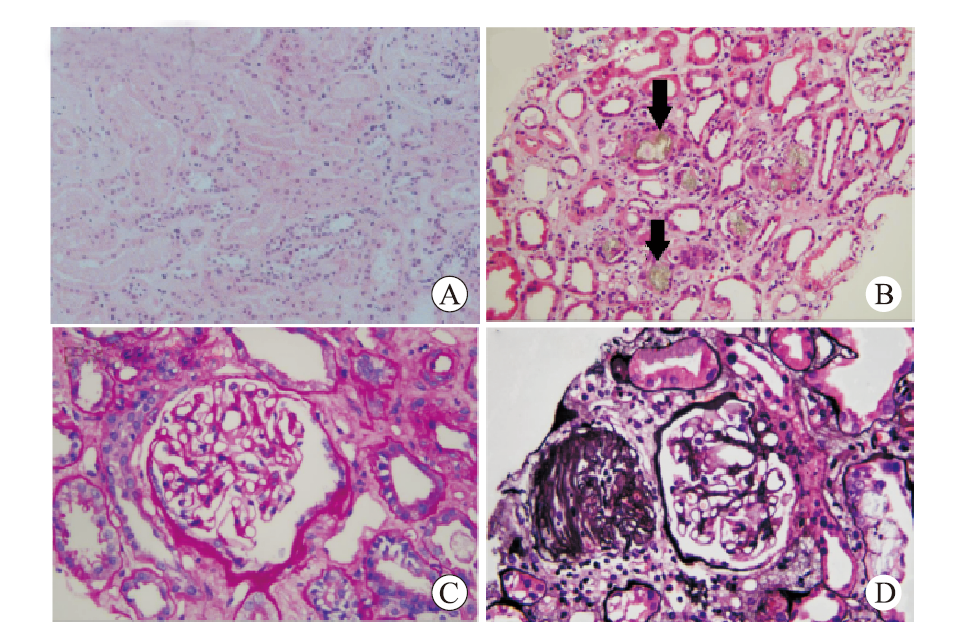
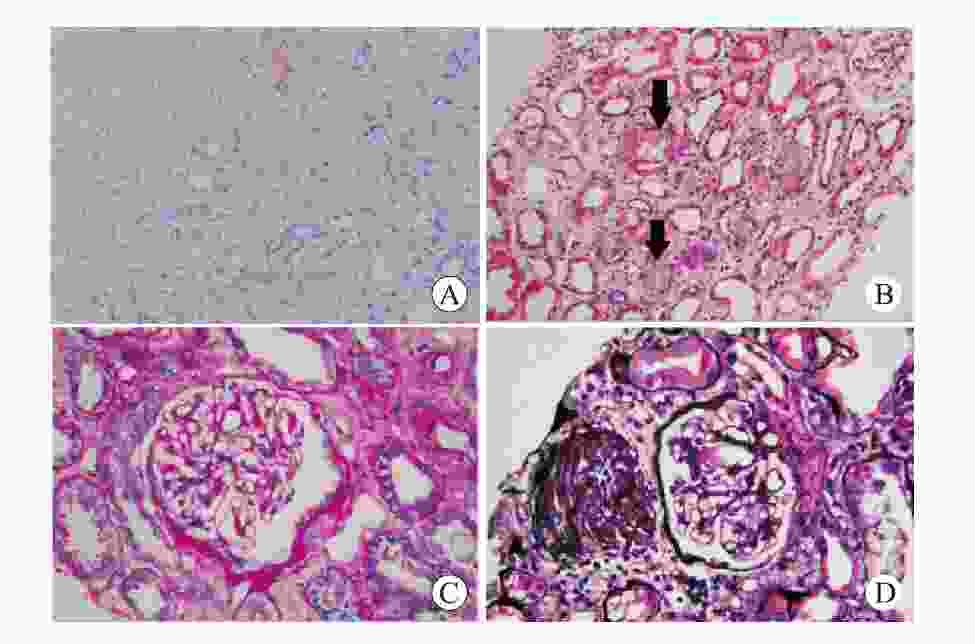
目的 总结肾移植术后腺嘌呤磷酸核糖基转移酶缺乏症的诊疗经验。 方法 回顾性分析1例肾移植术后腺嘌呤磷酸核糖基转移酶缺乏症患者的临床资料,结合文献复习总结该病临床特点、诊断、治疗和预后。 结果 患者肾活组织检查显示多数肾小管管腔内可见盐类结晶沉积,偏振光阳性。经过别嘌醇、血液透析和抗结晶等治疗移植物功能逐渐恢复。术后随访1年,患者肾功能恢复良好。 结论 肾移植术后腺嘌呤磷酸核糖基转移酶缺乏症可能导致移植物功能恢复延迟或障碍,早发现、早诊断、早治疗可延缓疾病进展,改善功能。 -
关键词:
- 腺嘌呤磷酸核糖基转移酶缺乏症 /
- 肾移植 /
- 2,8-二羟基腺嘌呤 /
- 移植物功能延迟恢复 /
- 移植物功能障碍 /
- 基因检测 /
- 血液透析 /
- 别嘌醇
Abstract:Objective To summarize the diagnosis and treatment experience of adenine phosphoribosyltransferase deficiency after kidney transplantation. Methods Clinical data of 1 patient with adenine phosphoribosyltransferase deficiency after kidney transplantation were retrospectively analyzed. Clinical characteristics, diagnosis, treatment and prognosis of adenine phosphoribosyltransferase deficiency were summarized by literature review. Results Renal biopsy showed that salt crystallization was found in most renal tubule lumen and positive results were observed under polarized light microscopy. After allopurinol, hemodialysis and anti-crystallization treatment, the graft function was gradually recovered. After postoperative 1-year follow-up, the patient's renal function was properly recovered. Conclusions Adenine phosphoribosyltransferase deficiency after kidney transplantation may lead to delayed graft function or graft dysfunction. Early detection, diagnosis and treatment may delay disease progression and improve renal function. -
表 1 APRT缺乏症患者的诊断方法和临床结局
Table 1. Diagnostic methods and clinical outcomes of patients with APRT deficiency
研究者 年份
(年)肾移植
次数年龄(岁)/
性别分析方法 诊断
时间移植物
活检特点移植物
存活时间结局 基因检测 其他 Nanmoku K, et al[6] 2017 1 28/男 98密码子从TGG到TGA无义突变 移植物穿刺活检和红外光谱 移植后 术后7 d肾小管腔内的小晶体沉积 >3个月 肾功能稳定 Li J, et al[7]
20191 47/男 未进行基因检测 移植前受者原肾穿刺活检 移植前 18个肾小球中有15个球性硬化,肾小管腔、上皮细胞质、间质有多个黄褐色晶体,伴有巨细胞、明显的肾小管萎缩和弥漫性间质纤维化。晶体呈针状、杆状和菱形形状,在偏振光下双折射 >6个月 DGF 1 52/女 纯合子c.188G>A;p.Gly63Asp突变 移植物穿刺活检 移植后 弥漫性间质炎症和纤维化,有黄褐色、双折射的管内晶体 >12个月 DGF Kaartinen K, et al[9] 2014 2 63/男 c.188G>A,p.G63D纯合突变,甘氨酸变为天冬氨酸 第2次肾移植移植物穿刺活检 移植后 肾小球形态正常,无排斥反应,但广泛的急性肾小管损伤和小管内未知类型针状晶体阻塞 >11个月 第1次移植物丢失,第2次移植物功能障碍 Brilland B,
et al[10]2015 1 25/女 未进行基因检测 FTIR① 移植后 无排斥反应,但发现ATN伴典型2,8-DHA晶体的管内沉积或结晶肾病 >18个月 肾功能稳定 George SA, et al[11]
20171 41/女 未进行基因检测 FTIR 移植后 肾小管管腔和肾小管细胞胞浆中有大量棕色结晶,慢性肾小管间质性肾炎,肾间质存在病灶,并伴有异物巨细胞 −② 肾功能稳定 Bagai S,
et al[12]
2019
144/男 APRT基因外显子3反义突变 移植物穿刺活检 移植后 肾小球正常,存在多个浅棕色环状管内晶体,在偏光显微镜下可折射,周围有异物巨细胞反应。免疫荧光显微镜检查结果阴性 >2个月 移植物功能障碍 Rajput P,
et al[13]
20201 43/男 外显子1(c.3G>C;
p.Met1)致病突变移植物穿刺活检 移植后 小管呈红棕色晶体 >2个月 移植物功能障碍 1 31/男 未进行基因检测 移植物穿刺活检 移植后 小管和间质呈红棕色晶体 >2个月 移植物功能障碍 注:①FTIR为傅里叶变换红外光谱。
②−为无数据。 -
[1] HUYET J, OZEIR M, BURGEVIN MC, et al. Structural insights into the forward and reverse enzymatic reactions in human adenine phosphoribosyltransferase[J]. Cell Chem Biol, 2018, 25(6): 666-676. DOI: 10.1016/j.chembiol.2018.02.011. [2] 宋远明, 赵长永, 李道兵. 遗传性代谢缺陷所致肾结石研究进展[J]. 浙江大学学报(医学版), 2023, 52(2): 169-177. DOI: 10.3724/zdxbyxb-2022-0698.SONG YM, ZHAO CY, LI DB. Research progress on renal calculus associate with inborn error of metabolism[J]. J Zhejiang Univ (Med Sci), 2023, 52(2): 169-177. DOI: 10.3724/zdxbyxb-2022-0698. [3] 刘宇坤, 葛玉成, 詹睿超, 等. 与嘌呤代谢相关的单基因肾结石病的研究进展[J]. 中华泌尿外科杂志, 2022, 43(2): 156-160. DOI: 10.3760/cma.j.cn112330-20211008-00531.LIU YK, GE YC, ZHAN RC, et al. Advances of monogenic kidney stone diseases associated with purine metabolism[J]. Chin J Urol, 2022, 43(2): 156-160. DOI: 10.3760/cma.j.cn112330-20211008-00531. [4] CEBALLOS-PICOT I, SAHA A, ARORA N, et al. Adenine phosphoribosyltransferase deficiency due to novel mutation[J]. Kidney Int Rep, 2018, 4(4): 624-628. DOI: 10.1016/j.ekir.2018.12.004. [5] HORINO T, ISHIHARA M, FUJIEDA M. Urinary 2, 8-dihydroxyadenine crystals in a patient with adenine phosphoribosyltransferase deficiency[J]. QJM, 2023, 116(10): 855-856. DOI: 10.1093/qjmed/hcad124. [6] NANMOKU K, KUROSAWA A, SHINZATO T, et al. Febuxostat for the prevention of recurrent 2, 8-dihydroxyadenine nephropathy due to adenine phosphoribosyltransferase deficiency following kidney transplantation[J]. Intern Med, 2017, 56(11): 1387-1391. DOI: 10.2169/internalmedicine.56.8142. [7] LI J, SHINGDE M, NANKIVELL BJ, et al. Adenine phosphoribosyltransferase deficiency: a potentially reversible cause of CKD[J]. Kidney Int Rep, 2019, 4(8): 1161-1170. DOI: 10.1016/j.ekir.2019.04.021. [8] RASHID I, VERMA A, TIWARI P, et al. Adenine phosphoribosyl transferase deficiency leads to renal allograft dysfunction in kidney transplant recipients: a systematic review[J]. J Bras Nefrol, 2022, 44(3): 403-416. DOI: 10.1590/2175-8239-JBN-2021-0283en. [9] KAARTINEN K, HEMMILÄ U, SALMELA K, et al. Adenine phosphoribosyltransferase deficiency as a rare cause of renal allograft dysfunction[J]. J Am Soc Nephrol, 2014, 25(4): 671-674. DOI: 10.1681/ASN.2013090960. [10] BRILLAND B, AUGUSTO JF, CROUE A, et al. A rare case of primary non-function of renal allograft due to adenine phosphoribosyltransferase deficiency[J]. Int Urol Nephrol, 2015, 47(9): 1589-1591. DOI: 10.1007/s11255-015-1077-y. [11] GEORGE SA, AL-RUSHAIDAN S, FRANCIS I, et al. 2, 8-Dihydroxyadenine nephropathy identified as cause of end-stage renal disease after renal transplant[J]. Exp Clin Transplant, 2017, 15(5): 574-577. DOI: 10.6002/ect.2015.0096. [12] BAGAI S, KHULLAR D, BANSAL B. Rare crystalline nephropathy leading to acute graft dysfunction: a case report[J]. BMC Nephrol, 2019, 20(1): 428. DOI: 10.1186/s12882-019-1616-3. [13] RAJPUT P, VIRANI ZA, SHAH BV. Crystalline nephropathy due to aprt deficiency: a preventable cause of renal and renal allograft failure[J]. Indian J Nephrol, 2020, 30(4): 290-292. DOI: 10.4103/ijn.IJN_106_19. [14] BALASUBRAMANIAM GS, ARENAS-HERNANDEZ M, ESCUREDO E, et al. Adenine phosphoribosyltransferase deficiency in the United Kingdom: two novel mutations and a cross-sectional survey[H]. Clin Kidney J, 2016, 9(6): 800-806. DOI: 10.1093/ckj/sfw093. [15] CHENG Y, GUO L, WANG M, et al. Recurrence of 2, 8-dihydroxyadenine crystalline nephropathy in a kidney transplant recipient: a case report and literature review[J]. Intern Med, 2021, 60(16): 2651-2657. DOI: 10.2169/internalmedicine.6640-20. [16] KUNOU M, YAMAGUCHI M, TAKAHASHI H, et al. A case of 2, 8-DHA crystalline nephropathy caused by adenine phosphoribosyltransferase deficiency: diagnosis and treatment[J]. CEN Case Rep, 2023, 12(3): 329-334. DOI: 10.1007/s13730-022-00768-1. [17] YAMAZAKI K, MIYAZAWA K, NIDA Y, et al. Rapidly progressive kidney dysfunction and crystal casts associated with adenine phosphoribosyltransferase (APRT) deficiency-lessons for the clinical nephrologist[J]. J Nephrol, 2021, 34(6): 2147-2149. DOI: 10.1007/s40620-021-01042-w. [18] SHIMOYAMA K, KANZAKI G, OKUBO A, et al. Foreign body granuloma with crystals, recurrent kidney stones, in a patient with adenine phosphoribosyltransferase deficiency[J]. QJM, 2023, 116(7): 536-537. DOI: 10.1093/qjmed/hcad037. [19] CHONG SL, NG YH. Obstructive uropathy and severe acute kidney injury from renal calculi due to adenine phosphoribosyltransferase deficiency[J]. World J Pediatr, 2016, 12(2): 243-245. DOI: 10.1007/s12519-015-0073-8. [20] NAJAFIAN B, LUSCO MA, ALPERS CE, et al. Approach to kidney biopsy: core curriculum 2022[J]. Am J Kidney Dis, 2022, 80(1): 119-131. DOI: 10.1053/j.ajkd.2021.08.024. [21] CHOY B, NAYAR R, LIN X. Role of renal mass biopsy for diagnosis and management: review of current trends and future directions[J]. Cancer Cytopathol, 2023, 131(8): 480-494. DOI: 10.1002/cncy.22697. [22] 米爱红, 高瑞瑞, 戴毅, 等. 超声引导下经皮肾穿刺活检在慢性肾脏病诊断中的价值[J]. 中国实验诊断学, 2023, 27(7): 808-810. DOI: 10.3969/j.issn.1007-4287.2023.07.014.MI AH, GAO RR, DAI Y, et al. The value of ultrasound-guided percutaneous renal biopsy in the diagnosis of chronic kidney disease[J]. Chin J Lab Diagn, 2023, 27(7): 808-810. DOI: 10.3969/j.issn.1007-4287.2023.07.014. [23] SINKS A, MILLER C, HOLCK H, et al. Renal mass biopsy mandate is associated with change in treatment decisions[J]. J Urol, 2023, 210(1): 72-78. DOI: 10.1097/JU.0000000000003429. [24] CHUNG R, KURTZMAN JT, GILLESPIE A, et al. The utility of renal mass biopsy in shared decision-making for renal mass treatment[J]. Urology, 2023, 178: 98-104. DOI: 10.1016/j.urology.2023.04.023. [25] BERTRAM A, BROECKER V, LEHNER F, et al. Kidney transplantation in a patient with severe adenine phosphoribosyl transferase deficiency: obstacles and pitfalls[J]. Transpl Int, 2010, 23(9): e56-e58. DOI: 10.1111/j.1432-2277.2010.01128.x. [26] DOLEŽELOVÁ E, KLEJCH T, ŠPAČEK P, et al. Acyclic nucleoside phosphonates with adenine nucleobase inhibit Trypanosoma brucei adenine phosphoribosyltransferase in vitro[J]. Sci Rep, 2021, 11(1): 13317. DOI: 10.1038/s41598-021-91747-6. [27] VALAPERTA R, RIZZO V, LOMBARDI F, et al. Adenine phosphoribosyltransferase (APRT) deficiency: identification of a novel nonsense mutation[J]. BMC Nephrol, 2014, 15: 102. DOI: 10.1186/1471-2369-15-102. [28] RUNOLFSDOTTIR HL, PALSSON R, AGUSTSDOTTIR IM, et al. Kidney disease in adenine phosphoribosyltransferase deficiency[J]. Am J Kidney Dis, 2016, 67(3): 431-438. DOI: 10.1053/j.ajkd.2015.10.023. [29] SINGH A, RAMACHANDRAN R, CHANDRALEKHA C, et al. Timing of intraoperative crystalloid infusion may decrease total volume of infusate without affecting early graft function in live related renal transplant surgery: a randomized, surgeon-blinded clinical study[J]. Indian J Urol, 2022, 38(1): 53-61. DOI: 10.4103/iju.iju_239_21. [30] DONG Y, SILVER SM, STERNS RH. Estimating urine volume from the urine creatinine concentration[J]. Nephrol Dial Transplant, 2023, 38(4): 811-818. DOI: 10.1093/ndt/gfab337. [31] OHYAMA T, SAKA N, TSUJIMOTO Y. Is allopurinol administration really effective in renal transplant patients?[J]. Transpl Immunol, 2022, 75: 101700. DOI: 10.1016/j.trim.2022.101700. [32] BOLLÉE G, DOLLINGER C, BOUTAUD L, et al. Phenotype and genotype characterization of adenine phosphoribosyltransferase deficiency[J]. J Am Soc Nephrol, 2010, 21(4): 679-688. DOI: 10.1681/ASN.2009080808. [33] BOLLÉE G, HARAMBAT J, BENSMAN A, et al. Adenine phosphoribosyltransferase deficiency[J]. Clin J Am Soc Nephrol, 2012, 7(9): 1521-1527. DOI: 10.2215/CJN.02320312. [34] YASEEN W, AUGUSTE B, ZIPURSKY J. Allopurinol hypersensitivity syndrome[J]. CMAJ, 2023, 195(13): E483. DOI: 10.1503/cmaj.221575. [35] MOHAMMAD CM, SHAHIDAH CA, WAN FATIMAH SWM, et al. Delayed hypersensitivity reaction to allopurinol: a case report[J]. Malays Fam Physician, 2023, 18: 11. DOI: 10.51866/cr.65. [36] HUONG PT, HA TN, NHU TTQ, et al. Allopurinol-induced Stevens-Johnson syndrome and toxic epidermal necrolysis: signal detection and preventability from Vietnam National pharmacovigilance database[J]. J Clin Pharm Ther, 2022, 47(12): 2014-2019. DOI: 10.1111/jcpt.13740. [37] BATHINI L, GARG AX, SONTROP JM, et al. Initiation dose of allopurinol and the risk of severe cutaneous reactions in older adults with CKD: a population-based cohort study[J]. Am J Kidney Dis, 2022, 80(6): 730-739. DOI: 10.1053/j.ajkd.2022.04.006. [38] EDVARDSSON VO, RUNOLFSDOTTIR HL, THORSTEINSDOTTIR UA, et al. Comparison of the effect of allopurinol and febuxostat on urinary 2, 8-dihydroxyadenine excretion in patients with adenine phosphoribosyltransferase deficiency (APRTd): a clinical trial[J]. Eur J Intern Med, 2018, 48: 75-79. DOI: 10.1016/j.ejim.2017.10.007. -




 下载:
下载: