Clinical outcome of kidney transplantation from DBD donors complicated with acute kidney injury
-
摘要:
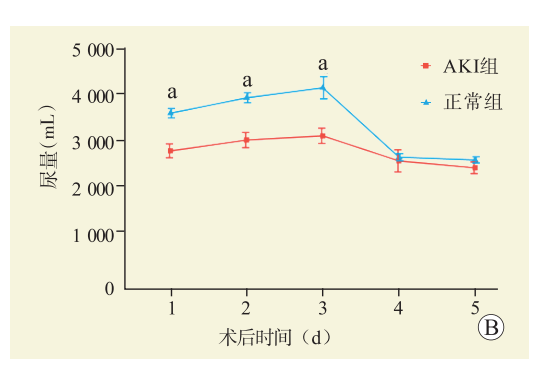
目的 探讨伴急性肾损伤(AKI)的脑死亡器官捐献(DBD)供者供肾肾移植的临床结局。 方法 回顾性分析216例DBD供者的资料,按照改善全球肾脏病预后组织(KDIGO)标准将分为AKI组(69例)与正常组(147例),AKI组进一步分为KDIGO 1期和2~3期两组,AKI组受者135例,正常组受者288例。总结受者术后肾功能恢复情况及临床结局。分析移植物功能延迟恢复(DGF)发生的危险因素。 结果 AKI组供者血清肌酐(Scr)最高值、获取前Scr值、血钠最高值、获取前血钠值均高于正常组,升压药物应用时间长于正常组,48 h内液体复苏用量高于正常组,入院HCO3−值低于正常组,尿崩症、低血压发生率高于对照组;KDIGO 2~3期供者Scr最高值、获取前Scr值较KDIGO 1期供者高(均为P<0.05)。与正常组比较,AKI组受者DGF、急性排斥反应发生率较高,行连续性肾脏替代治疗的比例较高,术后90 d内Scr水平较高,术后3 d尿量较少;与KDIGO 1期受者比较,KDIGO 2~3期受者术后3、4、5、15 d Scr水平较高,术后2 d尿量较少(均为P<0.05)。单因素分析结果显示供者年龄、Scr最高值、血钠最高值、48 h内液体复苏用量是肾移植术后受者发生DGF的危险因素,多因素分析结果显示,供者年龄是肾移植术后受者发生DGF的独立危险因素(均为P<0.05)。 结论 伴AKI的DBD供者供肾用于肾移植,经过积极的器官维护可纠正AKI,对术后6个月移植物功能和存活率没有影响,可达到与非AKI供肾同样的效果,可作为扩大供肾来源。 Abstract:Objective To evaluate the clinical outcome of kidney transplantation from donation after brain death (DBD) donors complicated with acute kidney injury (AKI). Methods Clinical data of 216 DBD donors were retrospectively analyzed, and they were divided into the AKI group (n=69) and control group (n=147) according to the Kidney Disease: Improving Global Outcomes (KDIGO) guidelines. Donors in the AKI group were further divided into the KDIGO stage 1 and stage 2-3 subgroups. One hundred and thirty-five recipients were assigned into the AKI group and 288 recipients in the control group. Postoperative recovery of renal function and clinical outcomes of the recipients were recorded. The risk factors of delayed graft function (DGF) were identified. Results The highest serum creatinine (Scr) level, Scr level before procurement, the highest blood sodium level and blood sodium level before procurement in the AKI group were higher than those in the control group. The application duration of vasopressors in the AKI group was longer than that in the control group. In the AKI group, the amount of fluid resuscitation within 48 h was higher, the HCO3− level at admission was lower, and the incidence of diabetes insipidus and hypotension was higher than those in the control group. The highest Scr level and the Scr level before procurement in KDIGO stage 2-3 donors were significantly higher than those in KDIGO stage 1 counterparts (all P<0.05). Compared with the control group, the incidence of DGF and acute rejection was higher, the proportion of continuous renal replacement therapy was higher, the Scr level within postoperative 90 d was higher, and the urine amount within postoperative 3 d was less than those of recipients in the AKI group. Compared with KDIGO stage 1 recipients, KDIGO stage 2-3 recipients had higher Scr levels at postoperative 3, 4, 5 and 15 d, and less urine amount at postoperative 2 d (all P<0.05). Univariate analysis showed that donor age, the highest Scr level, the highest blood sodium level and the amount of fluid resuscitation within 48 h were the risk factors for DGF in recipients after kidney transplantation. Multivariate analysis showed that donor age was the independent risk factor for DGF in recipients after kidney transplantation (all P<0.05). Conclusions For the application of DBD donors complicated with AKI, active organ maintenance should be performed to alleviate AKI. It exerts no effect upon graft function and survival rate at postoperative 6 months, which may achieve equivalent efficacy as non-AKI donors and may be used as a source of extended criteria donor kidneys. -
表 1 两组供者一般资料比较
Table 1. Comparison of general information of donors between two groups
指标 AKI组
(n=69)正常组(n=147) 统计值 P值 KDIGO 1期(n=43) KDIGO 2~3期(n=26) 统计值 P值 性别男[n(%)] 63(91) 125(85) 1.636 0.201 39(91) 24(92) 0.053 1.000 年龄[M(P25,P75),岁] 46(42,54) 50(43,56) 1.501 0.133 45(41,45) 49(41,54) −0.310 0.757 身高[M(P25,P75),cm] 172(170,176) 170(167,175) −2.080 0.038 172(170,178) 172(170,176) −0.638 0.523 体质量[M(P25,P75),kg] 75(68,80) 70(65,75) −3.011 0.003 75(65,80) 75(70,80) −0.559 0.576 BMI[M(P25,P75),kg/m2] 25(23,26) 24(22,26) −2.222 0.085 25(22,26) 25(23,26) −0.923 0.356 既往病史[n(%)] 高血压 28(41) 57(39) 0.064 0.800 20(47) 8(31) 1.665 0.197 糖尿病 6(9) 6(4) 0.205 3(7) 3(12) 0.425 0.665 心脏病 2(3) 1(1) 0.240 1(2) 1(4) 0.133 1.000 死亡原因[n(%)] 1.683 0.794 3.500 0.321 颅脑外伤 23(33) 54(37) 14(33) 9(35) 脑出血 37(54) 75(51) 23(53) 14(54) 脑梗塞 4(6) 9(6) 4(9) 0 缺血缺氧性脑病 5(7) 7(5) 2(5) 3(12) 其他 0 2(1) 0 0 发病至器官获取时间[M(P25,P75),d] 5(3,8) 5(3,7) −0.766 0.444 5(3,8) 5(4,6) −0.093 0.926 Scr最高值[M(P25,P75),µmol/L] 161(128,212) 67(53,82) −11.358 <0.001 137(117,160) 243(192,299) −6.496 <0.001 获取前Scr值[M(P25,P75),µmol/L] 98(73,107) 53(40,68) −8.525 <0.001 91(68,102) 102(81,117) −2.348 0.019 血钠最高值[M(P25,P75),mmol/L] 158(151,166) 145(140,151) −7.296 <0.001 158(151,165) 159(150,168) −0.217 0.828 获取前血钠值[M(P25,P75),mmol/L] 145(138,151) 139(135,145) −3.556 <0.001 145(138,151) 143(138,150) −0.192 0.848 升压药应用时间[M(P25,P75),d] 4.0(0,7.0) 0(0,3.0) −4.737 <0.001 3.0(0,7.0) 4.0(0.8,7.0) −0.848 0.397 48 h内液体复苏用量
($\overline x\pm s $,mL)9 701±2 686 6 961±2 233 −7.869 <0.001 9 369±2 111 10 250±3 410 −1.328 0.189 入院时HCO3—($\overline x\pm s $,mmol/L) 20±5 22±5 3.577 <0.001 20±4 19±6 −0.746 0.458 获取前HCO3—($\overline x\pm s $,mmol/L) 22(18,25) 21(18,24) −0.741 0.459 22(18,25) 21(17,26) −0.292 0.770 尿崩症[n(%)] 38(55) 46(31) 11.173 <0.001 26(60) 12(46) 1.341 0.247 低血压[n(%)] 47(68) 53(36) 19.415 <0.001 27(63) 20(77) 1.490 0.222 表 2 两组肾移植受者临床资料比较
Table 2. Comparison of clinical data of kidney transplant recipients between two groups
指标 AKI组(n=135) 正常组(n=288) 统计值 P值 KDIGO 1期(n=85) KDIGO 2~3期(n=50) 统计值 P值 性别男[n(%)] 104(77.0) 223(77.4) 0.008 0.928 68(80) 36(72) 1.139 0.286 年龄[M(P25,P75),岁] 39(32,47) 40(32,47) −0.562 0.574 39(33,47) 39(31,47) −0.716 0.474 身高[M(P25,P75),cm] 170(165,174) 170(165,174) −0.547 0.584 170(165,173) 170(162,175) −0.628 0.530 体质量[M(P25,P75),kg] 62(56,72) 66(56,74) −1.386 0.166 61(57,70) 68(55,73) −0.654 0.513 BMI[M(P25,P75),kg/m2] 22(20,24) 22(20,25) −1.034 0.301 22(20,24) 22(20,24) −0.868 0.385 移植前Scr值($\overline x\pm s $,µmol/L) 852±203 830±193 1.0756 0.283 移植前尿量($\overline x\pm s $,mL/d) 239±95 247±91 −0.890 0.374 热缺血时间($\overline x\pm s $,min) 2.8±0.9 2.8±1.1 −0.374 0.708 冷缺血时间($\overline x\pm s $,h) 4.0±1.9 3.9±1.8 0.570 0.568 6个月移植肾存活[n(%)] 130(96.3) 279(96.9) 0.901 0.390 80(94) 50(100) 1.849 0.291 12个月时失功[n(%)] 14(10.4) 28(9.7) 0.055 0.814 10(12) 4(8) 0.577 0.448 DGF[n(%)] 55(40.7) 87(30.2) 4.471 0.034 30(35) 25(50) 2.820 0.093 急性排斥反应[n(%)] 16(11.9) 12(4.2) 8.783 0.003 8(9) 8(16) 1.308 0.253 感染[n(%)] 7(5.2) 6(2.1) 0.127 4(5) 3(6) 0.710 CRRT[n(%)] 29(21.5) 33(11.5) 7.382 0.007 15(18) 14(28) 2.001 0.157 PNF[n(%)] 4(3.0) 4(1.4) 0.274 4(5) 0 0.296 谵妄[n(%)] 8(5.9) 11(3.8) 0.921 0.337 5(6) 3(6) 1.000 表 3 移植物功能延迟恢复的危险因素分析
Table 3. Analysis of risk factors of delayed graft function
项目 单因素分析 多因素分析 比值比 95%可信区间 P值 比值比 95%可信区间 P值 供者年龄 1.035 1.016~1.054 <0.001 1.045 1.024~1.065 <0.001 供者BMI 1.000 0.942~1.062 0.999 供者Scr最高值 1.003 1.000~1.006 0.023 1.002 0.999~1.005 0.266 供者血钠最高值 1.023 1.006~1.041 0.010 1.027 1.004~1.050 0.018 供者升压药应用时间 0.986 0.916~1.061 0.707 供者48 h内液体复苏用量 1.089 1.009~1.175 0.028 1.035 0.945~1.135 0.459 供者入院HCO3− 1.024 0.982~1.068 0.265 供者尿崩症 1.037 0.686~1.568 0.863 供者低血压 0.844 0.563~1.267 0.414 -
[1] TANNOUS LA, WESTPHAL GA, IOSHII SO, et al. Histological, laboratorial, and clinical benefits of an optimized maintenance strategy of a potential organ donor-a rabbit experimental model[J]. Life (Basel), 2023, 13(7): 1439. DOI: 10.3390/life13071439. [2] 谢良波, 夏秋翔, 曾宪鹏, 等. 《移植器官质量与安全指南(第6版)》解读——供者及器官的评估和选择标准[J]. 器官移植, 2020, 11(4): 487-491. DOI: 10.3969/j.issn.1674-7445.2020.04.011.XIE LB, XIA QX, ZENG XP, et al. Interpretation of Guide to the Quality and Safety of Organs for Transplantation (6th edition): evaluation and selection criteria for donors and organs[J]. Organ Transplantation, 2020, 11(4): 487-491. DOI: 10.3969/j.issn.1674-7445.2020.04.011. [3] NITA GE, GOPAL JP, KHAMBALIA HA, et al. Kidney transplantation from donors with acute kidney injury: are the concerns justified? a systematic review and meta-analysis[J]. Transpl Int, 2023, 36: 11232. DOI: 10.3389/ti.2023.11232. [4] 国家卫生健康委员会脑损伤质控评价中心, 中华医学会神经病学分会神经重症协作组, 中国医师协会神经内科医师分会神经重症专业委员会. 中国成人脑死亡判定标准与操作规范(第二版)[J]. 中华医学杂志, 2019, 99(17): 1288-1292. DOI: 10.3760/cma.j.issn.0376-2491.2019.17.003.Brain Injury Evaluation Quality Control Center of National Health and Family Planning Commission, Neurology Critical Care Cooperative Group of Neurology Branch of Chinese Medical Association, Neurology Critical Care Professional Committee of Neurology Physicians Branch of Chinese Medical Doctor Association. Criteria and practical specification for determination of brain death in adults (2nd edition)[J]. Natl Med J China, 2019, 99(17): 1288-1292. DOI: 10.3760/cma.j.issn.0376-2491.2019.17.003. [5] CHAWLA LS, BELLOMO R, BIHORAC A, et al. Acute kidney disease and renal recovery: consensus report of the Acute Disease Quality Initiative (ADQI) 16 Workgroup[J]. Nat Rev Nephrol, 2017, 13(4): 241-257. DOI: 10.1038/nrneph.2017.2. [6] KELLUM JA, LAMEIRE N, KDIGO AKI Guideline Work Group. Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (part 1)[J]. Crit Care, 2013, 17(1): 204. DOI: 10.1186/cc11454. [7] SONNENBERG EM, HSU JY, COHEN JB, et al. Acute kidney injury in deceased organ donors and kidney transplant outcomes: a national cohort study using a novel data source[J]. Ann Surg, 2022, 276(6): e982-e990. DOI: 10.1097/SLA.0000000000004597. [8] 王会龙, 阮东丽, 刘克普, 等. 扩大标准肾移植术后临床效果分析和器官维护策略探讨[J/OL]. 实用器官移植电子杂志, 2023, 11(2): 128-133. DOI: 10.3969/j.issn.2095-5332.2023.02.007.WANG HL, RUAN DL, LIU KP, et al. Clinical effect analysis and organ maintenance strategy investigation for expanded standard DCD renatransplantation[J/OL]. Pract J Organ Transplant (Electr Vers), 2023, 11(2): 128-133. DOI: 10.3969/j.issn.2095-5332.2023.02.007. [9] ANDERSON DJ, LOCKE JE. Progress towards solving the donor organ shortage[J]. Nat Rev Nephrol, 2023, 19(2): 83-84. DOI: 10.1038/s41581-022-00664-y. [10] XU H, HE X. Developments in kidney xenotransplantation[J]. Front Immunol, 2024, 14: 1242478. DOI: 10.3389/fimmu.2023.1242478. [11] 赵婕, 霍枫, 赵洪涛, 等. 系统性多科室协作器官捐献国际经验对我国的启示[J]. 器官移植, 2022, 13(6): 683-689. DOI: 10.3969/j.issn.1674-7445.2022.06.001.ZHAO J, HUO F, ZHAO HT, et al. Enlightenment of international experience of organ donation related systematic multi-department collaboration to China[J]. Organ Transplant, 2022, 13(6): 683-689. DOI: 10.3969/j.issn.1674-7445.2022.06.001. [12] HE W, WU Y, GONG C, et al. Contrast-enhanced ultrasonography for identifying acute kidney injury in brain-dead donors[J]. Quant Imaging Med Surg, 2023, 13(9): 6014-6025. DOI: 10.21037/qims-23-207. [13] WEBB CJ, MCCRACKEN E, JAY CL, et al. Single center experience and literature review of kidney transplantation from non-ideal donors with acute kidney injury: risk and reward[J]. Clin Transplant, 2023, 37(10): e15115. DOI: 10.1111/ctr.15115. [14] SRIVASTAVA V, NAKRA M, SHANKAR KA, et al. Optimal management of brain-dead organ donor[J]. Med J Armed Forces India, 2021, 77(1): 1-5. DOI: 10.1016/j.mjafi.2020.01.010. [15] YOUSIF ZK, KOOLA JD, MACEDO E, et al. Clinical characteristics and outcomes of drug-induced acute kidney injury cases[J]. Kidney Int Rep, 2023, 8(11): 2333-2344. DOI: 10.1016/j.ekir.2023.07.037. [16] LIU Q, ZHANG H, ZHONG M, et al. Excellent clinical outcomes of renal transplant from pediatric deceased donors with acute kidney injury[J]. Eur J Med Res, 2023, 28(1): 161. DOI: 10.1186/s40001-023-01111-9. [17] FIORENTINO M, BAGAGLI F, DELEONARDIS A, et al. Acute kidney injury in kidney transplant patients in intensive care unit: from pathogenesis to clinical management[J]. Biomedicines, 2023, 11(5): 1474. DOI: 10.3390/biomedicines11051474. [18] LEE MH, JEONG EG, CHANG JY, et al. Clinical outcome of kidney transplantation from deceased donors with acute kidney injury by Acute Kidney Injury Network criteria[J]. J Crit Care, 2014, 29(3): 432-437. DOI: 10.1016/j.jcrc.2013.12.016. [19] KIM KD, LEE KW, KIM SJ, et al. Safety and effectiveness of kidney transplantation using a donation after brain death donor with acute kidney injury: a retrospective cohort study[J]. Sci Rep, 2021, 11(1): 5572. DOI: 10.1038/s41598-021-84977-1. [20] 王红宇, 焦宪法, 牛杏果, 等. 伴急性肾损伤的脑死亡器官捐献供者供肾移植治疗的体会[J]. 器官移植, 2017, 8(6): 424-429. DOI: 10.3969/j.issn.1674-7445.2017.06.003.WANG HY, JIAO XF, NIU XG, et al. Experience of clinical efficacy of renal transplantation from donors of donation after brain death complicated with acute kidney injury[J]. Organ Transplant, 2017, 8(6): 424-429. DOI: 10.3969/j.issn.1674-7445.2017.06.003. [21] WESTPHAL GA, COLL E, DE SOUZA RL, et al. Positive impact of a clinical goal-directed protocol on reducing cardiac arrests during potential brain-dead donor maintenance[J]. Crit Care, 2016, 20(1): 323. DOI: 10.1186/s13054-016-1484-1. [22] 王红宇, 曲青山, 梁韶峰, 等. 自发性脑出血致脑死亡器官捐献供体脏器功能维护71例总结[J]. 国际医药卫生导报, 2018, 24(21): 3246-3247. DOI: 10.3760/cma.j.issn.1007-1245.2018.21.009.WANG HY, QU QS, LIANG SF, et al. Maintenance of 71 brain dead organ donation donors caused by spontaneous cerebral hemorrhage[J]. Inter Med Health Guid New, 2018, 24(21): 3246-3247. DOI: 10.3760/cma.j.issn.1007-1245.2018.21.009. [23] WESTPHAL GA, ROBINSON CC, GIORDANI NE, et al. Evidence-based checklist to delay cardiac arrest in brain-dead potential organ donors: the DONORS cluster randomized clinical trial[J]. JAMA Netw Open, 2023, 6(12): e2346901. DOI: 10.1001/jamanetworkopen.2023.46901. [24] 李爽, 包宇实. 缺血再灌注急性肾损伤机制研究进展[J]. 医学综述, 2020, 26(19): 3848-3853. DOI: 10.3969/j.issn.1006-2084.2020.19.020.LI S, BAO YS. Research progress in mechanisms of acute renal injury induced by ischemia-reperfusion injury[J]. Med Recap, 2020, 26(19): 3848-3853. DOI: 10.3969/j.issn.1006-2084.2020.19.020. [25] PUNUKOLLU R, RYAN M, MISRA S, et al. Past, current, and future perspectives on transplanting acute kidney injury kidneys[J]. Clin Pract, 2023, 13(4): 944-958. DOI: 10.3390/clinpract13040086. [26] DUARTE TTP, MAGRO MCS. Recovery of renal function in clinical patients with acute kidney injury: impact on mortality[J]. Life (Basel), 2022, 12(6): 852. DOI: 10.3390/life12060852. [27] WANG D, GUO Y, ZHANG Y, et al. Epidemiology of acute kidney injury in patients with stroke: a retrospective analysis from the neurology ICU[J]. Intern Emerg Med, 2018, 13(1): 17-25. DOI: 10.1007/s11739-017-1703-z. [28] HOUNKPATIN HO, FRASER SDS, GLIDEWELL L, et al. Predicting risk of recurrent acute kidney injury: a systematic review[J]. Nephron, 2019, 142(2): 83-90. DOI: 10.1159/000497385. [29] GARNER M, JAY CL, SHARDA B, et al. Long-term outcomes of kidney transplantation from deceased donors with terminal acute kidney injury: single center experience and literature review[J]. Clin Transplant, 2023, 37(3): e14886. DOI: 10.1111/ctr.14886. [30] PALMISANO A, GANDOLFINI I, DELSANTE M, et al. Acute kidney injury (AKI) before and after kidney transplantation: causes, medical approach, and implications for the long-term outcomes[J]. J Clin Med, 2021, 10(7): 1484. DOI: 10.3390/jcm10071484. [31] YAQUB S, HASHMI S, KAZMI MK, et al. A comparison of AKIN, KDIGO, and RIFLE definitions to diagnose acute kidney injury and predict the outcomes after cardiac surgery in a South Asian cohort[J]. Cardiorenal Med, 2022, 12(1): 29-38. DOI: 10.1159/000523828. [32] GOYAL A, DANESHPAJOUHNEJAD P, HASHMI MF, et al. Acute kidney injury[M]. Treasure Island (FL): StatPearls Publishing, 2024. [33] HAMZIC-MEHMEDBASIC A, MACKIC M, REBIC D, et al. Acute kidney injury classifications in the prediction of in-hospital mortality and renal function non-recovery[J]. Mater Sociomed, 2023, 35(4): 304-308. DOI: 10.5455/msm.2023.35.304-308. [34] KIM JH, KIM YS, CHOI MS, et al. Prediction of clinical outcomes after kidney transplantation from deceased donors with acute kidney injury: a comparison of the KDIGO and AKIN criteria[J]. BMC Nephrol, 2017, 18(1): 39. DOI: 10.1186/s12882-017-0461-5. [35] 刘洵, 薛梅, 吴安石. RIFLE、AKIN和KDIGO标准预测肝移植术后早期死亡的准确性比较[J]. 器官移植, 2020, 11(3): 369-373,390. DOI: 10.3969/j.issn.1674-7445.2020.03.008.LIU X, XUE M, WU AS. Comparison of the accuracy of RIFLE, AKIN and KDIGO criteria in predicting early death after liver transplantation[J]. Organ Transplant, 2020, 11(3): 369-373,390. DOI: 10.3969/j.issn.1674-7445.2020.03.008. [36] 陈佳弘, 徐莹, 何松哲, 等. 肝移植术后早期急性肾损伤的危险因素分析[J]. 中华器官移植杂志, 2023, 44(5): 269-274. DOI: 10.3760/cma.j.cn421203-20221230-00343.CHEN JH, XU Y, HE SZ, et al. Risk factors for early acute kidney injury after classic orthotopic liver transplantation[J]. Chin J Organ Transplant, 2023, 44(5): 269-274. DOI: 10.3760/cma.j.cn421203-20221230-00343. [37] KOYAWALA N, PARIKH CR. A review of donor acute kidney injury and posttransplant outcomes[J]. Transplantation, 2020, 104(8): 1553-1559. DOI: 10.1097/TP.0000000000003144. [38] LIU C, ALASFAR S, REESE PP, et al. Trends in the procurement and discard of kidneys from deceased donors with acute kidney injury[J]. Am J Transplant, 2022, 22(3): 898-908. DOI: 10.1111/ajt.16920. -





 下载:
下载: