Predictive values of ALBI and EZ-ALBI scores for early survival of recipients with liver failure after liver transplantation
-
摘要:
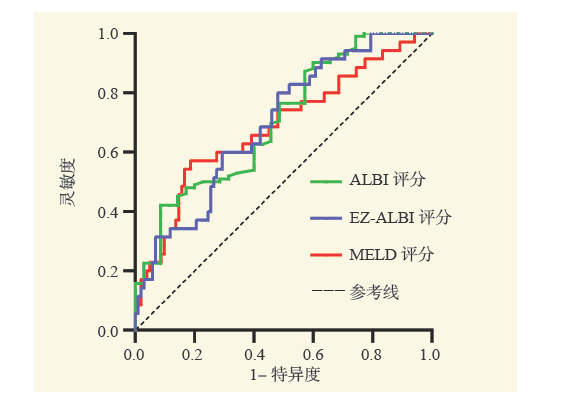
目的 探讨白蛋白-胆红素(ALBI)评分及简易白蛋白-胆红素(EZ-ALBI)评分对肝衰竭肝移植受者术后早期生存(术后3个月)的预测价值。 方法 回顾性分析确诊为肝衰竭并接受肝移植治疗的137例受者的临床资料。通过受试者工作特征(ROC)曲线下面积确定术前ALBI、EZ-ALBI和终末期肝病模型(MELD)评分预测肝衰竭肝移植受者术后早期生存的最佳截取值,采用单因素及多因素Cox回归分析肝衰竭肝移植受者术后早期死亡的危险因素,分析不同ALBI和EZ-ALBI水平对肝衰竭肝移植受者术后早期预后的影响。 结果 ALBI、EZ-ALBI和MELD评分的最佳截取值分别为0.21、-19.83和24.36,AUC分别为0.706、0.697和0.686。单因素Cox回归分析结果显示术前丙氨酸转氨酶(ALT)≥50 U/L、天冬氨酸转氨酶(AST)≥60 U/L、ALBI评分≥0.21和EZ-ALBI评分≥-19.83是肝衰竭肝移植受者术后早期死亡的危险因素(均为P < 0.05);多因素Cox回归分析结果显示术前ALBI评分≥0.21是肝衰竭肝移植受者术后早期死亡的独立危险因素(P < 0.05)。根据ALBI评分的最佳截取值进行分组,ALBI < 0.21组(46例)和ALBI≥0.21组(91例)的早期生存率分别为93.5%和64.8%,差异有统计学意义(P < 0.05);根据EZ-ALBI评分的最佳截取值进行分组,EZ-ALBI < -19.83组(60例)和EZ-ALBI≥-19.83组(77例)的早期生存率分别为88.3%和63.6%,差异有统计学意义(P < 0.05)。 结论 术前ALBI评分对于肝衰竭肝移植受者术后早期生存情况有良好的预测价值,可以作为选择肝移植受者的参考指标。 -
关键词:
- 肝移植 /
- 肝衰竭 /
- 白蛋白-胆红素(ALBI)评分 /
- 简易白蛋白-胆红素(EZ-ALBI)评分 /
- 受试者工作特征曲线 /
- 危险因素 /
- Child-Turcotte-Pugh(CTP)评分 /
- 终末期肝病模型(MELD)评分
Abstract:Objective To evaluate the predictive values of albumin-bilirubin (ALBI) and easy albumin-bilirubin (EZ-ALBI) scores for early survival (postoperative 3 months) of recipients with liver failure after liver transplantation. Methods Clinical data of 137 recipients diagnosed with liver failure and underwent liver transplantation were retrospectively analyzed. The optimal cut-off values of preoperative ALBI, EZ-ALBI and MELD scores to predict early survival of recipients with liver failure after liver transplantation were determined by the area under the receiver operating characteristic (ROC) curve. The risk factors of early death of recipients with liver failure after liver transplantation were identified by univariate and multivariate Cox regression analyses. The effects of different ALBI and EZ-ALBI levels upon early prognosis of recipients with liver failure after liver transplantation were analyzed. Results The optimal cut-off values of ALBI, EZ-ALBI and MELD scores were 0.21, -19.83 and 24.36, and the AUC was 0.706, 0.697 and 0.686, respectively. Univariate Cox regression analysis showed that preoperative alanine aminotransferase(ALT)≥50 U/L, aspartate aminotransferase(AST)≥60 U/L, ALBI score≥0.21 and EZ-ALBI score≥-19.83 were the risk factors for early postoperative death of recipients with liver failure after liver transplantation (all P < 0.05). Multivariate Cox regression analysis demonstrated that preoperative ALBI score≥0.21 was an independent risk factor for early postoperative death of recipients with liver failure after liver transplantation (P < 0.05). According to the optimal cut-off value of ALBI score, the early survival rates in the ALBI < 0.21 (n=46) and ALBI≥0.21(n=91) groups were 93.5% and 64.8%, and the difference was statistically significant (P < 0.05). According to the optimal cut-off value of EZ-ALBI score, the early survival rates in the EZ-ALBI < -19.83(n=60) and EZ-ALBI≥-19.83(n=77) groups were 88.3% and 63.6%, and the difference was statistically significant (P < 0.05). Conclusions Preoperative ALBI score is of high predictive value for early survival of recipients with liver failure after liver transplantation, which could be utilized as a reference parameter for selecting liver transplant recipients. -
表 1 肝衰竭肝移植受者术后早期死亡的危险因素分析
Table 1. Analysis of risk factors for early postoperative death in liver transplant recipients with liver failure
变量 单因素分析 多因素分析 HR①(95%CI②) P值 HR(95%CI) P值 一般资料 性别(男比女) 0.685(0.329~1.427) 0.312 -③ - 年龄(≥50岁比 < 50岁) 0.998(0.514~1.937) 0.996 - - 术前资料 HBsAg(阳性比阴性) 1.046(0.434~2.520) 0.920 - - PT(≥15 s比 < 15 s) 1.099(0.426~2.833) 0.845 - - ALT(≥50 U/L比 < 50 U/L) 2.484(1.216~5.073) 0.013 1.819(0.709~4.671) 0.214 AST(≥60 U/L比 < 60 U/L) 2.205(1.033~4.707) 0.041 0.990(0.360~2.722) 0.984 GGT(≥50 U/L比 < 50 U/L) 0.891(0.458~1.733) 0.735 - - ALB(≥35 g/L比 < 35 g/L) 0.730(0.371~1.436) 0.362 - - PLT(≥60×109 /L比 < 60×109 /L) 1.596(0.775~3.285) 0.205 - - TB(≥200 μmol/L比 < 200 μmol/L) 1.001(1.000~1.003) 0.070 血清肌酐(≥71 μmol/L比 < 71 μmol/L) 1.506(0.885~2.562) 0.131 血清钠(≥135 mmol/L比 < 135 mmol/L) 0.685(0.329~1.427) 0.313 - - ALBI评分(≥0.21比 < 0.21) 6.485(1.984~21.192) 0.002 4.518(1.034~19.747) 0.045 EZ-ALBI评分(≥-19.83比 < -19.83) 3.718(1.623~8.520) 0.002 1.287(0.449~3.688) 0.639 术中资料 手术时间(≥350 min比 < 350 min) 1.022(0.447~2.341) 0.958 - - 输液量(≥4 L比 < 4 L) 1.282(0.638~2.577) 0.486 - - 注:①HR为风险比。
②CI为可信区间。
③-为无数据。 -
[1] ZACCHERINI G, WEISS E, MOREAU R. Acute-on-chronic liver failure: definitions, pathophysiology and principles of treatment[J]. JHEP Rep, 2020, 3(1): 100176. DOI: 10.1016/j.jhepr.2020.100176. [2] ARROYO V, MOREAU R, JALAN R. Acute-on-chronic liver failure[J]. N Engl J Med, 2020, 382(22): 2137-2145. DOI: 10.1056/NEJMra1914900. [3] 黄敏, 李冬冬, 刘传苗. 乙肝相关慢加急性肝衰竭患者临床短期预后因素的分析[J]. 中华全科医学, 2021, 19(12): 2028-2030. DOI: 10.16766/j.cnki.issn.1674-4152.002227.HUANG M, LI DD, LIU CM. Analysis of clinical short-term prognostic factors in patients with hepatitis B-related acute-on-chronic liver failure[J]. Chin J Gen Pract, 2021, 19(12): 2028-2030. DOI: 10.16766/j.cnki.issn.1674-4152.002227. [4] CHANG J, MATHEJA A, KRZYCKI S, et al. Model for end-stage liver disease underestimates mortality of patients with acute-on-chronic liver failure waiting for liver transplantation[J]. Dig Liver Dis, 2022, 54(6): 784-790. DOI: 10.1016/j.dld.2021.12.011. [5] KARIYAMA K, NOUSO K, HIRAOKA A, et al. EZ-ALBI score for predicting hepatocellular carcinoma prognosis[J]. Liver Cancer, 2020, 9(6): 734-743. DOI: 10.1159/000508971. [6] DEMIRTAS CO, D'ALESSIO A, RIMASSA L, et al. ALBI grade: evidence for an improved model for liver functional estimation in patients with hepatocellular carcinoma[J]. JHEP Rep, 2021, 3(5): 100347. DOI: 10.1016/j.jhepr.2021.100347. [7] GUO G, LEI Z, TANG X, et al. External validation of six liver functional reserve models to predict posthepatectomy liver failure after major resection for hepatocellular carcinoma[J]. J Cancer, 2021, 12(17): 5260-5267. DOI: 10.7150/jca.58726. [8] 中华医学会感染病学分会肝衰竭与人工肝学组, 中华医学会肝病学分会重型肝病与人工肝学组. 肝衰竭诊治指南(2018年版)[J]. 临床肝胆病杂志, 2019, 35(1): 38-44. DOI: 10.3969/j.issn.1001-5256.2019.01.007.Liver Failure and Artificial Liver Group of Chinese Society of Infectious Diseases of Chinese Medical Association, Severe Liver Disease and Artificial Liver Group of Chinese Society of Hepatology of Chinese Medical Association. Guideline for diagnosis and treatment of liver failure (2018)[J]. J Clin Hepatol, 2019, 35(1): 38-44. DOI: 10.3969/j.issn.1001-5256.2019.01.007. [9] 孙梦园, 向晓星. ALBI评分对肝硬化食管胃底静脉曲张破裂出血患者预后的预测价值[J]. 临床肝胆病杂志, 2021, 37(3): 590-595. DOI: 10.3969/j.issn.1001-5256.2021.03.017.SUN MY, XIANG XX. Value of albumin-bilirubin score in predicting the prognosis of cirrhotic patients with esophagogastric variceal bleeding[J]. J Clin Hepatol, 2021, 37(3): 590-595. DOI: 10.3969/j.issn.1001-5256.2021.03.017. [10] FAGENSON AM, GLEESON EM, PITT HA, et al. Albumin-bilirubin score vs model for end-stage liver disease in predicting post-hepatectomy outcomes[J]. J Am Coll Surg, 2020, 230(4): 637-645. DOI: 10.1016/j.jamcollsurg.2019.12.007. [11] LING Q, DAI H, ZHUANG R, et al. Predicting short-term survival after liver transplantation on eight score systems: a national report from China Liver Transplant Registry[J]. Sci Rep, 2017, 7: 42253. DOI: 10.1038/srep42253. [12] HUEBENER P, STERNECK MR, BANGERT K, et al. Stabilisation of acute-on-chronic liver failure patients before liver transplantation predicts post-transplant survival[J]. Aliment Pharmacol Ther, 2018, 47(11): 1502-1510. DOI: 10.1111/apt.14627. [13] MISE Y, VAUTHEY JN, ZIMMITTI G, et al. Ninety-day postoperative mortality is a legitimate measure of hepatopancreatobiliary surgical quality[J]. Ann Surg, 2015, 262(6): 1071-1078. DOI: 10.1097/SLA.0000000000001048. [14] THÜRING J, RIPPEL O, HAARBURGER C, et al. Multiphase CT-based prediction of Child-Pugh classification: a machine learning approach[J]. Eur Radiol Exp, 2020, 4(1): 20. DOI: 10.1186/s41747-020-00148-3. [15] VANDERWERKEN DN, WOOD NL, SEGEV DL, et al. The precise relationship between model for end-stage liver disease and survival without a liver transplant[J]. Hepatology, 2021, 74(2): 950-960. DOI: 10.1002/hep.31781. [16] CREEDEN JF, GORDON DM, STEC DE, et al. Bilirubin as a metabolic hormone: the physiological relevance of low levels[J]. Am J Physiol Endocrinol Metab, 2021, 320(2): E191-E207. DOI: 10.1152/ajpendo.00405.2020. [17] CHENG XP, ZHAO J, CHEN Y, et al. Comparison of the ability of the PDD-ICG clearance test, CTP, MELD, and MELD-Na to predict short-term and medium-term mortality in patients with decompensated hepatitis B cirrhosis[J]. Eur J Gastroenterol Hepatol, 2016, 28(4): 444-448. DOI: 10.1097/MEG.0000000000000538. [18] RUF A, DIRCHWOLF M, FREEMAN RB. From Child-Pugh to MELD score and beyond: taking a walk down memory lane[J]. Ann Hepatol, 2022, 27(1): 100535. DOI: 10.1016/j.aohep.2021.100535. [19] 都泓莲, 何鸿雁, 王波, 等. CTP分级评分联合吲哚菁绿清除试验对HBV相关性慢加急性肝衰竭患者短期预后的评估[J]. 实用医学杂志, 2020, 36(12): 1679-1683. DOI: 10.3969/j.issn.1006-5725.2020.12.026.DU HL, HE HY, WANG B, et al. Assessment of the predictive value of CTP grading score combined with the indocyanine green clearance test for short-term prognosis of acute-on-chronic hepatitis B liver failure[J]. J Pract Med, 2020, 36(12): 1679-1683. DOI: 10.3969/j.issn.1006-5725.2020.12.026. [20] FUNG J, MAK LY, CHAN AC, et al. Model for end-stage liver disease with additional criteria to predict short-term mortality in severe flares of chronic hepatitis B[J]. Hepatology, 2020, 72(3): 818-828. DOI: 10.1002/hep.31086. [21] POMMERGAARD HC, DAUGAARD TR, ROSTVED AA, et al. Model for end-stage liver disease score predicts complications after liver transplantation[J]. Langenbecks Arch Surg, 2021, 406(1): 55-65. DOI: 10.1007/s00423-020-02018-3. [22] TEH SH, SHEPPARD BC, SCHWARTZ J, et al. Model for end-stage liver disease score fails to predict perioperative outcome after hepatic resection for hepatocellular carcinoma in patients without cirrhosis[J]. Am J Surg, 2008, 195(5): 697-701. DOI: 10.1016/j.amjsurg.2007.05.054. [23] WAGENER G. Assessment of hepatic function, operative candidacy, and medical management after liver resection in the patient with underlying liver disease[J]. Semin Liver Dis, 2013, 33(3): 204-212. DOI: 10.1055/s-0033-1351777. [24] PINATO DJ, SHARMA R, ALLARA E, et al. The ALBI grade provides objective hepatic reserve estimation across each BCLC stage of hepatocellular carcinoma[J]. J Hepatol, 2017, 66(2): 338-346. DOI: 10.1016/j.jhep.2016.09.008. [25] MARASCO G, ALEMANNI LV, COLECCHIA A, et al. Prognostic value of the albumin-bilirubin grade for the prediction of post-hepatectomy liver failure: a systematic review and Meta-analysis[J]. J Clin Med, 2021, 10(9): 2011. DOI: 10.3390/jcm10092011. [26] LI MX, ZHAO H, BI XY, et al. Prognostic value of the albumin-bilirubin grade in patients with hepatocellular carcinoma: validation in a Chinese cohort[J]. Hepatol Res, 2017, 47(8): 731-741. DOI: 10.1111/hepr.12796. [27] HIRAOKA A, KUMADA T, HIROOKA M, et al. A better method for assessment of hepatic function in hepatocellular carcinoma patients treated with radiofrequency ablation: usefulness of albumin-bilirubin grade[J]. Hepatol Res, 2018, 48(3): E61-E67. DOI: 10.1111/hepr.12927. [28] 赵首捷, 杨振宇, 雷世雄, 等. Child-Pugh评分和ALBI分级对BCLC-B期肝癌生存预后预测价值比较[J/CD]. 中华肝脏外科手术学电子杂志, 2021, 10(1): 38-42. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHZW202101009.htmZHAO SJ, YANG ZY, LEI SX, et al. Comparison of prognostic value between Child-Pugh score and albumin-bilirubin grading for patients with BCLC-B stage hepatocellular carcinoma[J/CD]. Chin J Hepat Surg(Electr Edit), 2021, 10(1): 38-42. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHZW202101009.htm [29] 王哲轩, 王恩鑫, 夏冬东, 等. Child-Pugh评分和ALBI分级预测经肝动脉化疗栓塞治疗不可切除肝细胞癌预后的价值比较[J]. 临床肝胆病杂志, 2020, 36(1): 113-117. DOI: 10.3969/j.issn.1001-5256.2020.01.025.WANG ZX, WANG EX, XIA DD, et al. Value of Child-Pugh score versus albumin-bilirubin grade in predicting the prognosis of unresectable hepatocellu-lar carcinoma treated by transarterial chemoembolization[J]. J Clin Hepatol, 2020, 36(1): 113-117. DOI: 10.3969/j.issn.1001-5256.2020.01.025. [30] FENG R, KAN K, STICHT C, et al. A hierarchical regulatory network ensures stable albumin transcription under various pathophysiological conditions[J]. Hepatology, 2022, DOI: 10.1002/hep.32414[Epubahead of print]. [31] NÚÑEZ KG, SANDOW T, PATEL J, et al. Hypoalbuminemia is a hepatocellular carcinoma independent risk factor for tumor progression in low-risk bridge to transplant candidates[J]. Cancers (Basel), 2022, 14(7): 1684. DOI: 10.3390/cancers14071684. -





 下载:
下载: